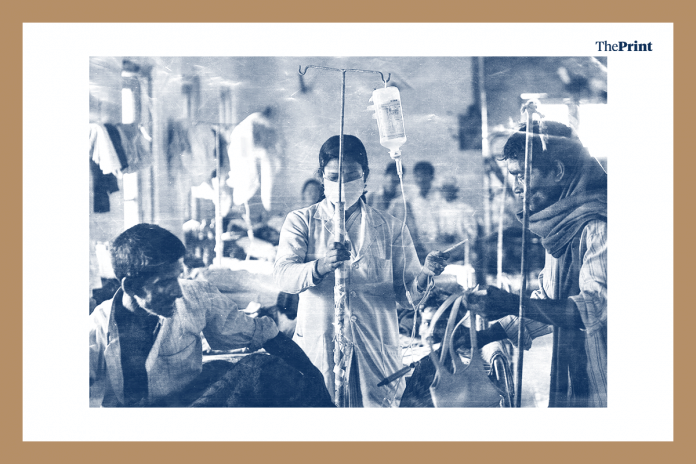
Data shows that India has only one doctor for every 11,000 patients, and one hospital for more than 55,000 people.
WHO prescribes a doctor-patient ratio of 1:1000. To meet the same, India would need at least 5 lakh more doctors.
ThePrint asks: Is India’s abysmal doctor-patient ratio a self-made crisis?
Realistic HR policies, affordable college fees can bring more doctors into public health system
 Keshav Desiraju
Keshav Desiraju
Former health secretary
The success of Ayushman Bharat depends on its ability to provide comprehensive primary health care to communities. India has 492 medical colleges out of which 233 are government-owned, offering more than 62,960 MBBS seats. This is a large number but the perceived scarcity is because most doctors are not in the public health system.
At the postgraduate level, the distribution of specialisations is skewed, with the ’lucrative’ options — radiology, orthopaedics and gynaecology — being preferred over family medicine, geriatric care, psychiatry. To get more doctors into the public system, we need more government colleges with affordable fees. Doctors passing out of private colleges will not come to government hospitals because they cannot afford to as they have to recover their training costs. All government colleges must offer postgraduate courses in under-represented disciplines.
State governments need to put in place realistic, workable HR policies, which will ensure that doctors posted in difficult areas stay at their posts. We cannot rely on the doctors’ sense of duty or their professional ethics to keep them in such areas.
Doctors alone do not constitute a public health system. We need more government nursing colleges, trained midwives and nurses. We have an abundance of AYUSH doctors, who must be drawn into the public health system, provided they work only within their disciplines and not as substitute allopaths.
Most doctors work in metros, rural India is at the mercy of pseudo-chemist
 Shailaja Chandra
Shailaja Chandra
Retired civil servant and former secretary in the health ministry
India’s shortage of doctors is colossal. This is because the Indian Medical Council Act only allows a person enrolled in the allopathic medical register to practice allopathy. No one else can treat using allopathic drugs scheduled under the Drugs Act 1940. Notwithstanding the easy availability of most over-the-counter drugs, the law forbids prescriptions and treatment by any non-enrolled medical practitioner.
For decades, this artificial gap has been filled by lakhs of non-allopathic practitioners, AYUSH doctors, chemists, and even quacks. According to a 2016 WHO report, the prevalence of unqualified practitioners outnumbered that of regular doctors in India.
Another aberration is that all doctors, whether allopathic or AYUSH, work only in the metros, Tier I and II cities, and towns where a paying clientele is available. In India’s six lakh villages, medical treatment is provided by the nearest unqualified practitioner, pseudo-chemist or traditional healers.
In a recent research paper, we have advocated that licensing medical practitioners, who have undergone training in a medical college or a district hospital, is critically needed for providing medical treatment to rural households. Alternately, nurse, midwives, or paramedics already working in rural areas need to be trained and allowed to provide basic medical treatment for day-to-day illnesses.
The government proposal to authorise nurse practitioners to treat illnesses through a legal amendment in the National Medical Commission Bill is truly welcome. It can be a game-changer. There is a critical short supply of nurse practitioners “with specialisation in tertiary nursing and ICU care and cardiac problems”. Such highly trained practitioners would never give up hospital-based work to attend to village households.
Community-based providers must be selected locally, trained, enrolled and then licensed to provide limited allopathic treatment in rural areas. The licentiate medical practitioner (LMP) was very much a part of India’s rural health workforce before the MCI was established in 1956. LMPs seriously need to be reinvented to replace lakhs of quacks who are dangerous and provide irrational treatment to ignorant rural communities.
Existing medical hierarchy, gender insensitivity need to be addressed
 Meera Shiva
Meera Shiva
Public health activist
A large percentage of our population is neglected by comprehensive primary healthcare. Investment in health, especially public health, has been unfortunate. The inadequate number of doctors, nurses, lab technicians as well as concentration of doctors in urban areas highlight the inequity in India’s healthcare.
Nurse practitioners have delivered on care with competence, when armed with good training, standard operating procedures, back-up of essential diagnostics and medicines, referral services as well as mechanisms to seek medical advice if needed. Women health visitors and experienced auxiliary nurse midwives have delivered maternal and other care in rural areas.
Many doctors do not want to go to rural areas because of the working conditions there and the availability of greener pastures elsewhere in the country and abroad. There have been community programmes in the 1970s and 1980s wherein nurses provided healthcare. Gender and social sensitivity was a part of such programmes.
There is no doubt that many people need medical care, especially the marginalised and those suffering from multiple vulnerabilities. They have been denied that for very long. With the increasing burden of chronic non-communicable diseases, malnutrition, maternal and reproductive health problems, much more needs to be done.
Nurse-practitioners along with the requisite support system will definitely be able to contribute. The existing medical hierarchy and gender insensitivity needs to be acknowledged and addressed sensitively.
Not rational to expect doctors to uphold ‘public service perspective’ in the absence of essential services
 Himani Chandna
Himani Chandna
Special Correspondent, ThePrint
Engineering seats outnumber the MBBS seats by 22:1. The All India Council for Technical Education (AICTE) has been successful in creating a regular supply of engineers but failed to meet the requirement for doctors. Most of these doctors prefer urban area postings, leading to another challenge of uneven distribution of medical experts.
The skewed distribution of doctors has led to an urban-rural doctor density of 3.8:1, as per the Niti Aayog. Roughly, three in four primary care visits are fee-charging private providers, of whom 57.3 per cent do not have a required medical qualification.
But let’s not assume that a doctor is a diabolical creature. From living in a pest-infested accommodation and surviving without basic amenities like electricity, life security or drinking water, hospitals in rural areas are sometimes a nightmare for doctors.
It may not be rational to expect doctors to uphold ‘public service perspective’ in the absence of essential medicines, ambulance services, and basic life-saving infrastructure.
If the system does not generate as many doctors as required, it must also know how to effectively utilise their expertise.
For instance, our country has over seven lakh AYUSH doctors and 1.92 lakh BDS degree holders — this number takes the medical workforce to nearly 20 lakh doctors.
With a strong health infrastructure, the government could train another cadre of doctors who could take up the responsibility of primary healthcare, thereby, allowing MBBS doctors to take care of larger, specialised roles.
Compiled by Deeksha Bhardwaj, journalist at ThePrint.






Ok Mr editor first of all Ur asking questions to wrong persons…what wud a health secretary or a civil service person know when they are not specialist in this field..this is the reason for downgrading healthcare..beaurocrats and politicians have eaten away the health of India…if healthcare policy will be made by these uneducated NETAS and general ias individuals whiteout any specialist knowledge this is bound to happen..what India needs is ALL INDIA MEDICAL SERVICES WITH COMPLETE AUTIONIMY TO DOCTORS REPORTING TO PRIME MINISTER..then only this state of crisis can be solved..
I am a doctor. Governments, including state govt as well as central now hire doctors at a salary which can be equated to a high school teacher or a junior engineer and the appointment is contractual, devoid of any regular amenities. Then it (government) wants the doctors to perform social service of highest standards in lowest standards of living. Why a doctor would then go for a government job?