The world is beginning to loosen restrictions that have been put in place to limit the spread of Covid-19. Leaders of countries, states and cities are finding they have little choice but to return to economic activity well before an effective vaccine or treatment for the disease is available. This means secondary outbreaks are a near certainty.
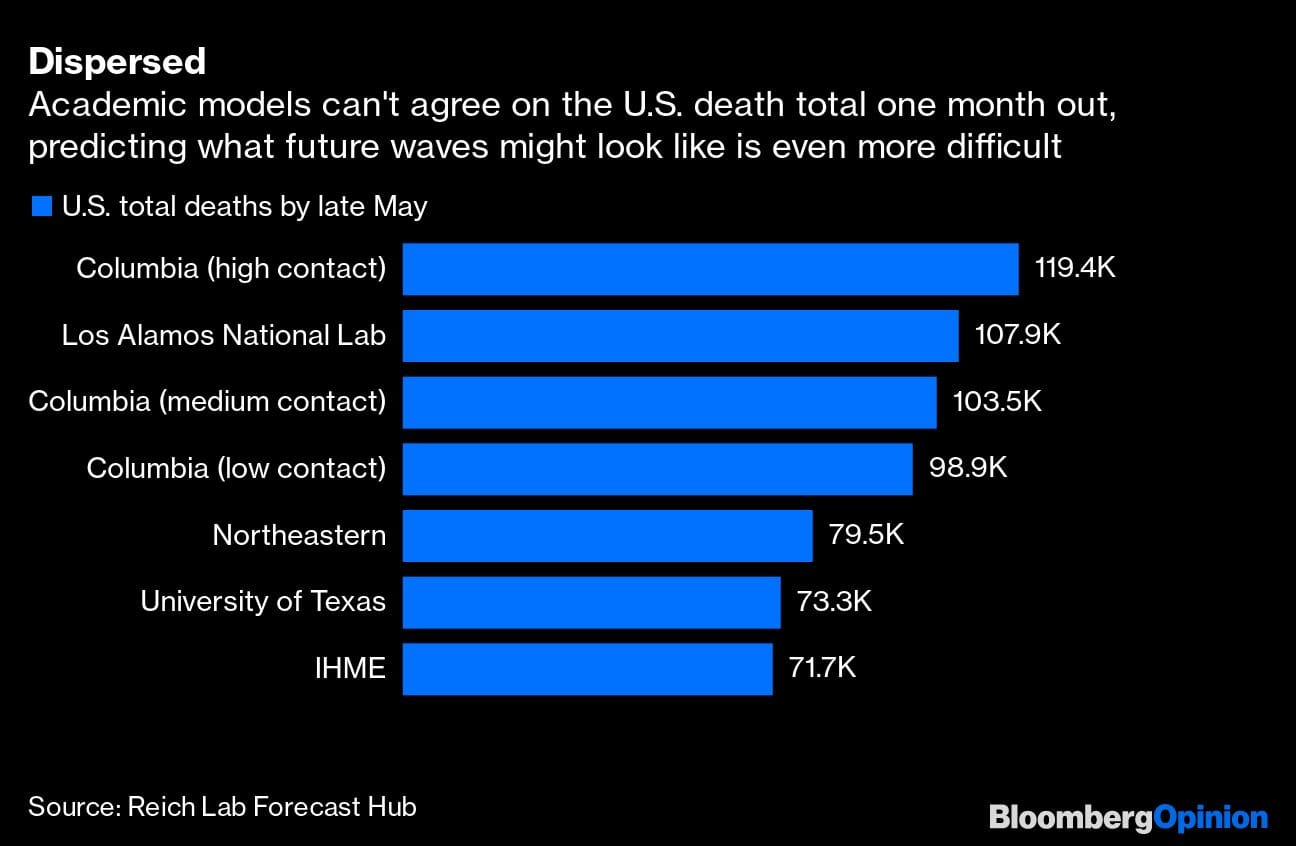
What’s uncertain is how devastating future surges of infection will be. If they’re sporadic and kept under control, death rates will stay low, and life may inch back toward normalcy. If they’re large, countries and regions may need to dive back into shutdown mode, extending the pandemic’s economic damage.
Unfortunately, many of the factors that will determine what’s coming are beyond anyone’s control.
That’s not to say countries are entirely powerless over their fates. Areas that open gradually and with widespread testing and contact-tracing programs will most easily be able to detect and interrupt outbreaks. But nature will play a significant role, too, and an unpredictable one — starting with the weather.
The coronavirus that causes Covid-19 might behave as the common coronaviruses that cause many mild respiratory infections do. They spread more readily in colder, drier environments and have a harder time infecting people when the weather is warm and humid. (They’re helped by the way people cram together indoors during cold weather.) In the U.S., these viruses typically peak in November and December and fall to a trough from February to May.
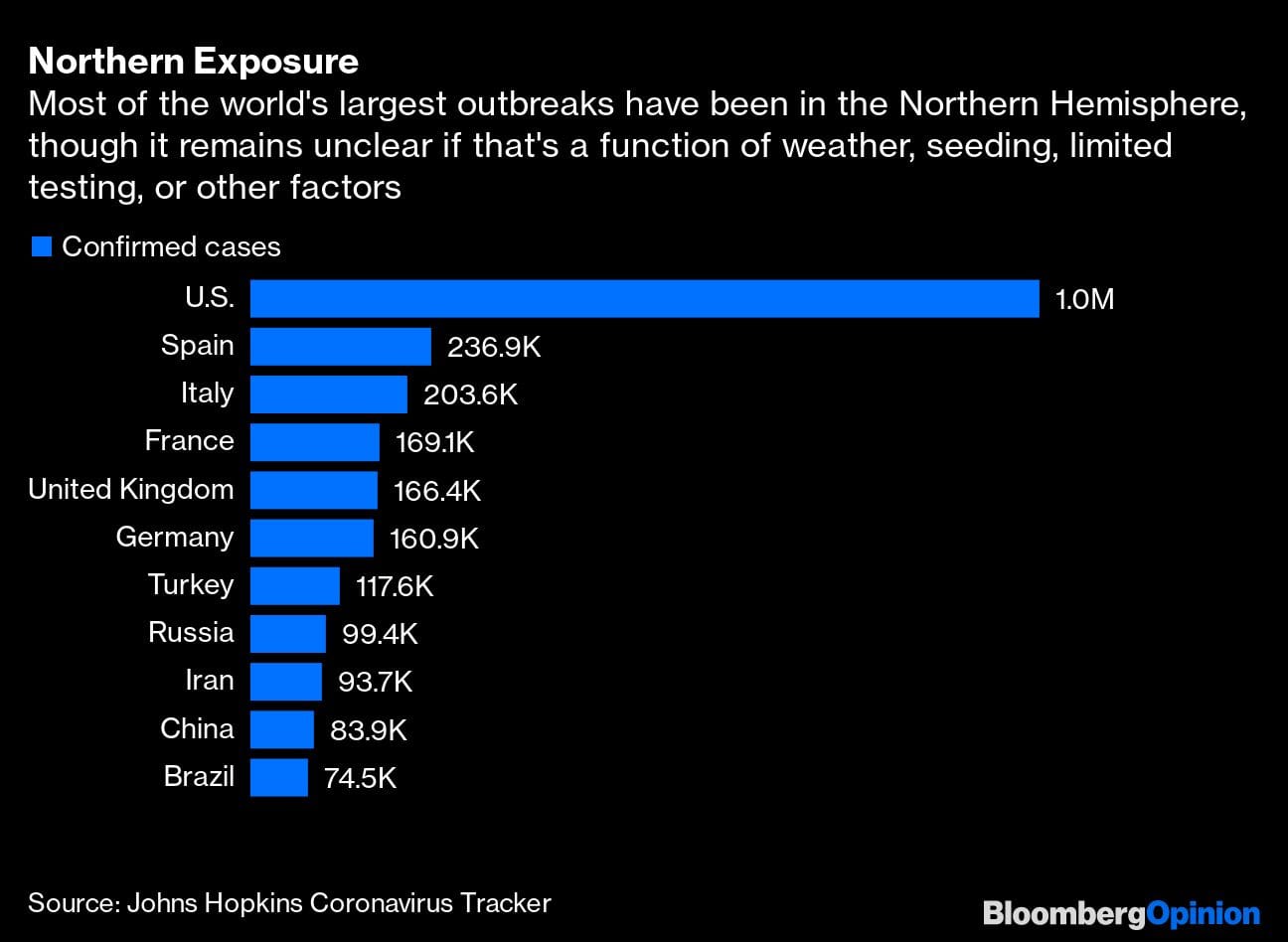
Medical scientists have yet to determine the extent to which seasonal tendencies apply to Covid-19. But any warm-weather decline this year is likely to arrive late and not amount to much. After all, the disease didn’t show up in many parts of the world until late winter. While there’s some evidence that this coronavirus doesn’t care for heat, most transmission has been occurring indoors. And the existence of outbreaks in warmer nations (Thailand and Singapore, for instance) and the sheer virulence of Covid-19 suggest that dramatic summer suppression is unlikely.
Seasonality may nevertheless at least limit the size of any post-lockdown rebound. New outbreaks in the Northern Hemisphere this summer could be smaller, and that would buy valuable time to make progress on testing, developing treatments and reinforcing health systems. On the other hand, it could also mean that the virus begins to spread more rapidly in the Southern Hemisphere, and that later outbreaks in the fall and winter will be especially acute in places where people neglect to take appropriate precautions.
Theoretically, the coronavirus might also peter out, as viruses do, if populations acquire immunity and it runs out of people to infect. While most countries around the world have either embraced social distancing or invested aggressively in containment, Sweden has imposed only mild restrictions. Its goal is to reduce the economic impact of the pandemic. Racing toward “herd immunity” isn’t an explicit aim of the policy, according to the country’s chief epidemiologist, but it’s a helpful threshold he thinks could be achieved in Stockholm within weeks.
The problem with this strategy, beyond its potentially high human cost, is that scientists know little about acquired immunity to Covid-19. Contracting a virus generally leads to some future protection, as the body’s immune system remembers the bug and is prepared with antibodies for the next fight. However, the duration and strength of this immunity varies by the disease, the intensity of the person’s infection, and other factors. There have been reports of people infected with the Covid virus twice — though these might reflect testing problems. But resistance to seasonal coronaviruses is known to fade within a year. And while antibodies to SARS, Covid-19’s cousin, have lasted longer, the SARS outbreak died out before researchers had a chance to observe whether they broadly prevent reinfection. Months-long studies of antibody-positive individuals are needed to learn about acquired immunity to Covid-19.
Thus, Sweden is taking its chances. And it’s not clear it would be a good idea for any country to issue “immunity passports” for people who test positive for Covid-19 antibodies.
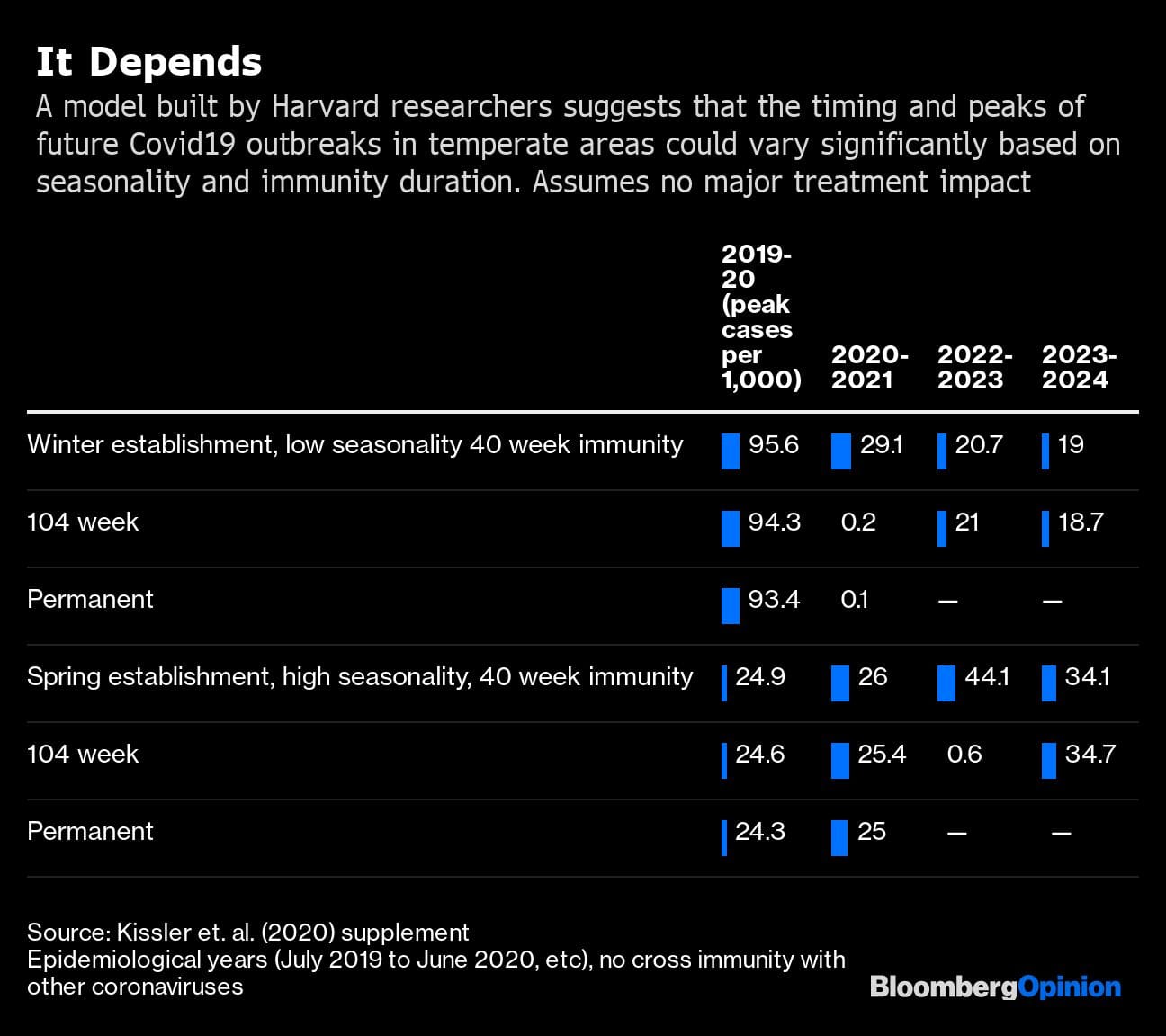
If it turns out that immunity is easily gained and long-lasting, infection rates should decline over time. If it’s transient and unreliable, the world could face annual or biennial outbreaks for years to come. One model of Covid-19’s future transmission dynamics suggests that the size of outbreaks will vary drastically depending on the virus’s seasonality and the duration of people’s immunity.
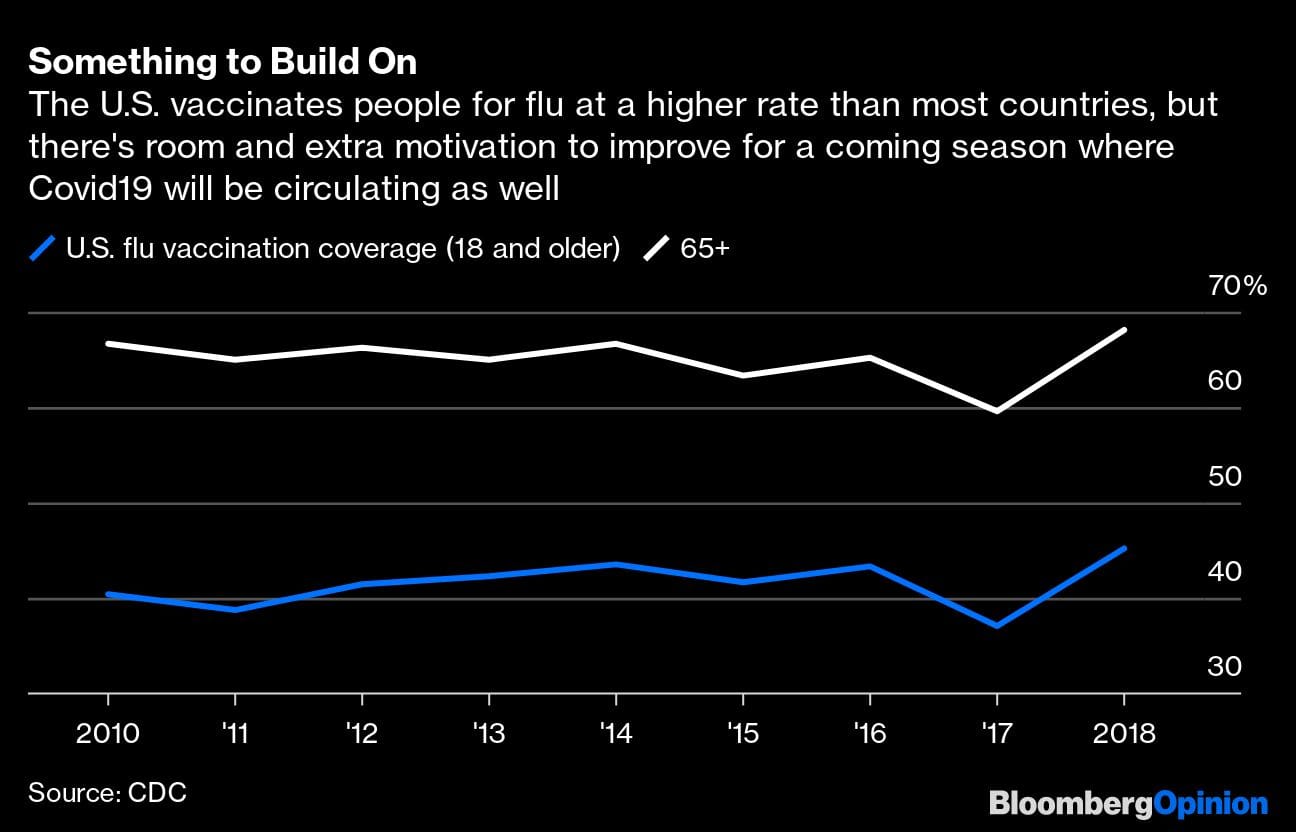
Going forward, countries have experience and, having flattened the curve, more time to prepare. Yet when cold weather returns in the fall, they may face a new challenge: the simultaneous return of Covid-19 and the flu. This could sow confusion and strain testing and hospital capacity. Robert Redfield, director of the U.S. Centers for Disease Control and Prevention, has noted that a winter outbreak of Covid-19 could be more troublesome even if it is smaller than the one we’re having now.
It will help if more of the world’s population gets a flu vaccine. In an average year, however, less than half of American adults do.
Scientific breakthroughs could also steer the trajectory of Covid-19: The discovery of an effective treatment would greatly reduce suffering and strain on health care systems. Wednesday’s news that Gilead Sciences Inc’s remdesivir sped recovery in some hospitalized patients in a placebo-controlled trial is welcome, even though it’s not the game changer that’s needed. And by the fall, scientists should have data on lab-grown antibodies that could potentially prevent and treat the disease. However, treatments and vaccines now in the works are aimed at the version of the coronavirus that is currently spreading. Any significant mutation could undermine progress.
In the face of so many unknowns, countries and companies have no choice but to approach reopening with all possible caution.
Also read: How China is attempting to prevent a second wave of infections






