As everyone celebrates the 50th anniversary of the Bangladesh Liberation War, there is a lesser known Indian achievement from 1971 that is saving lives even today — and not just in India. A humble Bengali doctor who worked tirelessly in the refugee camps along the India-Bangladesh border created one of the greatest health innovations that has saved over 70 million lives globally so far, most of them children.
Adversity is the mother of all inventions, and the adversity in the refugee camps during the 1971 war was that they had run out of intravenous fluid saline during a cholera epidemic. So Dr Dilip Mahalanabis, a paediatrician and a clinical scientist, relied on jugaad and with the help of Johns Hopkins International Center for Medical Research and Training created oral rehydration salt sachets or ORS.
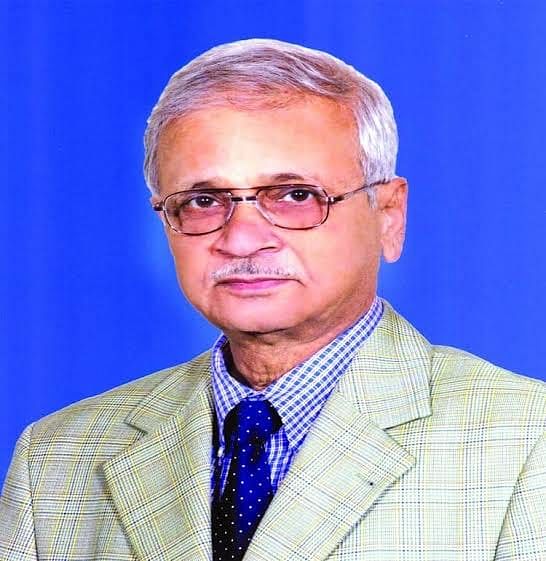
He is 86 today and lives in Kolkata, and still has not got due recognition from the Centre or state governments for pioneering the use of ORS for diarrhoeal diseases.
And even though everyone knows ORS, which Lancet called “potentially the most important medical advance” of the 20th century, not many remember Dr Dilip Mahalanabis.
Also read: 1971 to 2021 – We fought together, now Bangladesh Army marches with us on Republic Day
Miracle in a refugee camp
In 1971, millions of people from erstwhile East Pakistan (now Bangladesh) were rendered homeless and fled to India. They received shelter in numerous refugee camps set up on the India-Bangladesh border. In the absence of access to food, clean drinking water and proper sanitation, most of the refugees became prone to cholera, a water-borne infectious disease that causes diarrhoea leading to dehydration and even death.
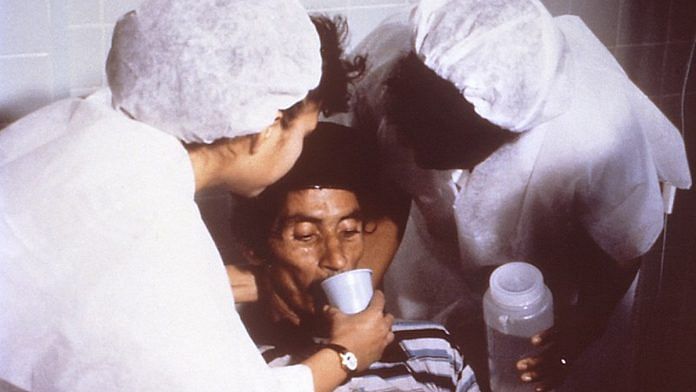
In one of the refugee camps in Bangaon in West Bengal, where Dilip Mahalanabis was on medical supervision, the situation turned worse when the intravenous fluid saline (the standard treatment till then) ran out. As the outbreak turned into an epidemic, the camps were also running out of trained medical staff too.
“There were two rooms in the hospital in Bangaon that were filled with severely ill cholera patients lying on the floor. In order to treat these people with IV saline, you literally had to kneel down in their faeces and their vomit. Within 48 hours of arriving there, I realized we were losing the battle because there was not enough IV and only two members of my team were trained to give IV fluids,” Mahalanabis later told the World Health Organization (WHO).
In this precarious situation, Mahalanabis, with support from the Johns Hopkins University Center for Medical Research and Training (JH-CMRT) in Calcutta took an innovative risk of using Oral Rehydration Therapy (ORT) for the people in the camp. The team working with him made ready-to-use ORT sachets or ORS consisting of a mixture of table salt (four teaspoons), baking soda (three teaspoons) and commercial glucose (20 teaspoons). Mothers, relatives, friends or anybody available in the camp were mobilised to give ORS to patients.
The desperation to save lives forced Mahalanabis to take the risk of starting this still-unrecommended treatment. Till then, the clinical trial of the efficacy of ORS was confined to the laboratory, far from being approved by the medical fraternity. Another doctor needs to be mentioned here — Hemendra Nath Chatterjee. He was the first Indian doctor who as early as in the 1950s used an oral glucose-sodium electrolyte solution closely similar to the modern-day ORS formulation to treat 186 cholera patients in Kolkata. However, because of inadequate methodology, his findings were not put to use by other clinicians/scientists.
The results of the ORS application were overwhelmingly reassuring. The death rate dropped from 30 per cent to 3.6 per cent in the hospitals under Dr Mahalanabis’ supervision within two weeks.
“We were just happy that it worked there and that we could help these people. We prepared pamphlets describing how to mix salt and glucose and distributed them along the border. The information was also broadcast on a clandestine Bangladeshi radio station,” he said.
Also read: Why India is home to millions of refugees but doesn’t have a policy for them
ORS can and does work
After its mass application and success in other refugee camps, the WHO adopted ORS in 1978 as its primary tool to fight cholera and childhood diarrhoea, and took up the project across 105 countries.
Today, if you are in any country around the equatorial belt, it is very likely that you have used 13.5 gm glucose, 2.6 gm sodium chloride, 2.9 gm trisodium citrate and 1.5 gm potassium chloride some time in your life. A sachet of this powder diluted in 1 litre of clean water has saved many from imminent death and is the most prescribed medicine for prevention of dehydration and management of acute diarrhoea, which still kills around 525,000 children under five annually. The total production of ORS across the globe is around 500 million sachets per year currently. With a cost-effective price of about Rs 20 per pack, India alone has a market of Rs 160 crore per year, which reflects the demand for this solution. In fact, every year, 29 July is observed as world ORS Day.
Dr Dhiman Barua, the Head of the Bacterial Diseases Unit of WHO in the 1970s and also Mahalanabis’ mentor, was convinced of the effectiveness of this low-cost medication. In an article, Mahalanabis shared that it was not him but Barua who “moved it from within WHO for a global initiative”. This journey was not easy. They had to struggle a lot to convince the medical fraternity that reversing dehydration can also be possible through oral rehydration with much lesser risk, and even without any medical supervision or support.
Subsequent studies have shown that timely use of ORS can successfully treat 80 per cent of cholera patients, both adults and children.
Also read: India boosts child vaccinations but lags in access to pneumonia & diarrhoea treatment — report
Reforming public health
For this remarkable contribution, in 1994, Mahalanabis was elected as a member of the Royal Swedish Academy of Sciences. He received the Pollin Prize from the US in 2002 and the Prince Mahidol Award from the government of Thailand in 2006. A graduate from Calcutta Medical College and Hospital, Mahalanabis studied cholera and other diarrhoeal diseases at the Johns Hopkins Center during 1966-70 and was associated with the WHO for a long period of time. He retired as the director of the International Centre for Diarrhoeal Diseases and Research, Dhaka in 1995.
It is surprising that someone who received such high acclaim globally, did not get enough recognition from his own country.
Despite the role of ORS in preventing diarrhoeal disease mortality, even today diarrhoea has been ranked 3 among the top 10 diseases leading to childhood illness and death. One of the key reasons for that is the under-implementation of the ORT, especially in the lower and lower-middle income countries where access to safe drinking water and sanitation is a serious challenge. As per the recently released National Family Health Survey-V report, none of the states is using ORS to its full potential for the treatment of diarrhoea. For example, in Bihar, while the prevalence of diarrhoea was 14 per cent in the two weeks preceding the survey period, only 58 per cent of these children had received ORS in this period; even the best-performing state in ORS usage, West Bengal, reported using the oral solution on only 75 per cent of diarrhoea-affected children.
It is never late to remember the person who revolutionised diarrhoea treatment even now and follow his goals. Perhaps the best tribute to Dr Mahalanabis would be a sound public health system that never falters on timely provisioning of basic and inexpensive solutions such as ORS.
The author works with Centre for Budget and Governance Accountability (CBGA), New Delhi. Views are personal.



Shame on everyone including WHO and Govt of India that we never knew about his achievement so far.
In India doctors are always painted in bad light by media, they say doctors have no right to make profit….. While everyone including the lawyers, journalist, and politicians have right to do corruption and Amass as much wealth as possible….
Thank you. Very good article on scientific advances.
So he is the one that gave a new life to these termites! Hop the present government is reading this article and gives this Doctor a well deserved Padma award.
Very inspiring story! At least, State Govt of Bengal could have given him due recognition and recommended him for Padma award along with Dr. Barua. Perhaps he remained out of India for a long time and therefore, went out of attention he deserved. But it is never too late. Our Health Minister or even PM should be told about his story. The country owes a lot of gratitude to Dr. Mahalanobis.