Muzaffarpur: It always begins the same way. High fever, convulsions and a child unable to rise from unconsciousness, often with symptoms of a cold or cough.
When Ramnath Sahni, a 38-year-old labourer from Muzaffarpur district noticed that his four-year-old son was shaking in his sleep, forehead burning to the touch, he picked him up in his arms and rushed him to Sri Krishna Medical College and Hospital (SKMCH) as quickly as possible. Sahni knows that children are dying because of “chamki bukhar” — as many as 89 have died this month in this very hospital — but he’s not sure what the cause or cure really is.
“I bought the medicine they asked me to, it cost me Rs 600, but I had no choice,” he tells ThePrint, fanning his son with his right hand as he holds up a makeshift mask to his face with his left.
“You claim to be a government hospital, but what facilities are you really providing here? The doctor came and looked at him once, said a drip will be put, and hasn’t returned since,” he says.

On another bed, Devanshi Kumar tells ThePrint the same story. Her four-year-old daughter Shanti Devi lies sideways next to her, tongue curling in and out of her mouth as if to vomit, but finding no food in her stomach to do so. Kumar removes the diaper around her daughter’s legs, revealing a trail of loose, watery stool that has begun to wet the bed-sheet.
“The doctors haven’t told us anything,” Kumar says.
Acute Encephalitis Syndrome (AES) — a neurological disorder characterised by the inflammation of the brain — has reared its ugly head in Muzaffarpur once more. As of 17 June, 312 patients were admitted in the district’s SKMCH due to AES affliction, with over 270 of them being under the age of 7, shows hospital data.
Nearly 110 have died in the district, including casualties at Kejriwal Matrisadan, another hospital in the area, reported The Indian Express.
Also read: Why 100 deaths from encephalitis have prompted Bihar to issue a lychee advisory
‘Unpredictable nature of AES’
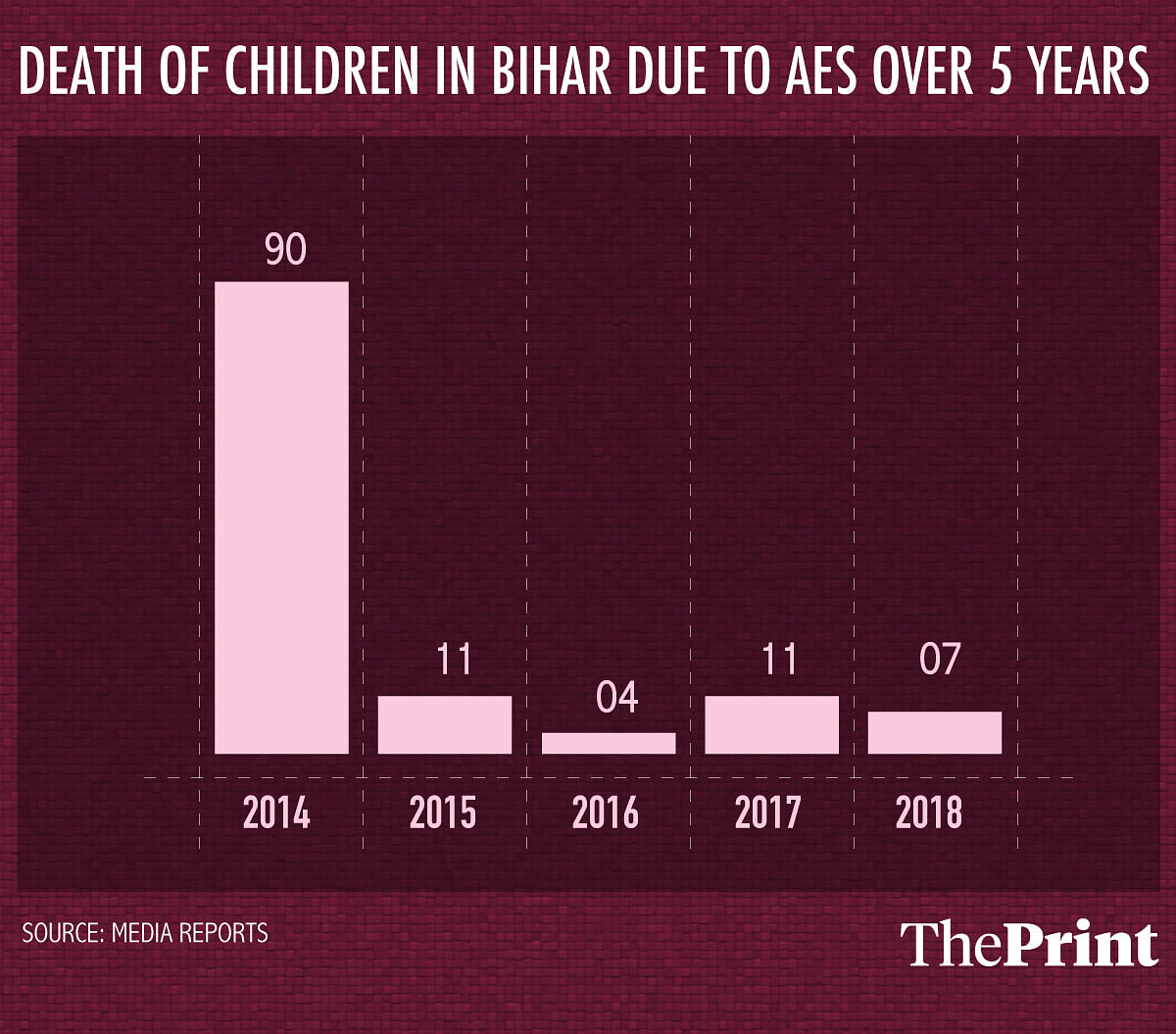
For a stable four years, the BIMARU state of Bihar had learnt how to contain AES’ insidious spread. Bihar’s health department data reportedly show that the disorder claimed the lives of 11 children in 2015, four in 2016, 11 in 2017 and seven in 2018 — a significant decrease from the reported 120 deaths in 2012 and 90 in 2014.
Now, in 2019, with reported deaths of over 100 children, doctors, medical experts and state officials appear to be fumbling with the disorder once more — seeking accountability in factors like heat, hypoglycaemia (low blood sugar levels) and the consumption of the litchi fruit.
Bihar’s Principal Health Secretary and IAS officer Sanjay Kumar even blames the “unpredictable nature of AES, which makes it very difficult to say why the numbers are up some years and down the next”.
“We don’t quite understand the ideology of the disease,” says Kumar.
What had been done
Bihar had learnt its lesson, only to unlearn it now.
A Standard Operating Procedure (SOP) was developed by the Bihar health department in accordance with UNICEF guidelines in 2015, following the previous year’s AES debacle.
The SOP mobilised Accredited Social Health Activists (ASHA) workers on a large scale, distributing pamphlets to targeted demographics on sanitation and nutritional practices. ASHA, as well as Anganwadi workers and auxiliary nurse-midwives (ANM) would distribute ORS packets during the summer months when temperatures spike. Surveys to identify at-risk families in villages were conducted, and provisions were also made for basic amenities in primary health centres.
The reclamation of Uttar Pradesh actually followed that of Bihar’s — in 2017, when over 500 children died of Japanese Encephalitis in Gorakhpur and its neighbouring regions, CM Yogi Adityanath was pushed against a wall. Under pressure, he pushed for early vaccination drives, wide-scale fogging, information campaigns, segregating pigs from affected areas, and informing parents of ambulance helpline numbers and the importance of sanitation.
It worked.
Deaths in the 14 most-affected districts in eastern Uttar Pradesh districts dropped by over 66 per cent in 2018 over the previous year.
By the time Adityanath woke up to the problem, Bihar had already controlled it. The initiatives placated the struggle, which is why when Union Minister of Health and Family Welfare Dr Harsh Vardhan failed to live up to his 2014 promise of setting up a virology laboratory in Muzaffarpur, no one really cared — and he could just make it again five years later.
But now AES is back, and the Modi government is sending researchers last minute to Muzaffarpur, Chief Minister Nitish Kumar has promised a Rs 4 lakh ex-gratia sum to each of the families and even personally visited the hospital Tuesday. The state government is scrambling to do damage control, while doctors are realising that they had merely snoozed the problem and not solved it.
Medical professionals who have seen AES through the decades in Bihar are still speaking in the terminology of ‘theory’, hypothesising various reasons for its sudden resurgence.
Also read: Now there’s an LED bulb to fight bacteria. Question is, do we really need it
Why now?
“Bihar also suffered from a disease called ‘Kala Azar (Black Fever)’,” Prabhat Kumar Sinha, former dean of research at the Indira Gandhi Institute of Medical Sciences in Patna, tells ThePrint.
“From 2014-16, there was a massive spray of DDT (a chemical compound) to kill sand-flies and mosquitoes. Now that the effectiveness of the spray has worn off, it’s possible these vectors have returned again,” he says, clarifying “but this is merely speculation, I’m not sure”.
Sinha also looks to contaminated water and lack of sanitation for answers. “Water-borne viruses, like the enterovirus, also found in North Vietnam, can make its way to shallow tube-wells, which is a feature of dry-summers since water levels decrease,” he suggests.
“This infected water can then impact young children, who are already malnourished and susceptible to illness. A lot of the cases this time had vomiting as a symptom, which suggests a prior infection to AES.”
For Gopal Shankar Sahni, the head of the paediatrics department in SKMCH, the “ceaseless humidity in Muzaffarpur and adjoining areas this year is the main culprit of this disease”.
“Compared to the preceding four years, 2019 is witnessing unbearable levels of humidity, which do not fluctuate under 60 per cent or get respite in the form of rain,” Sahni says. “What’s worse is the humidity only increases at night, if there was any change in levels, this wouldn’t have happened.”
Meanwhile, Dr Arun Shah, the president of the Bihar state branch of the Indian Academy of Paediatrics, is fielding a call from The New York Times when this reporter walks into his office. Outside the air-conditioned walls of his sprawling two-room office, in what Google Maps says is “Doctor Arun Shah Lane” in Bahranpura, Muzaffarpur, at least 30 patients await treatment in the heat.
He talks about his paper on AES at length, in which he and his colleague Dr T. Jacob John had found a link between litchi consumption by malnourished children and the onset of AES.
“Only malnourished children, impoverished, and the poorest of the poor suffer from this problem. It’s everything, from heat and humidity to sanitation, ignorance and finally, the litchi, which is only the triggering factor that affects these already predisposed children,” he says.
“We had suggested in 2016 in our paper that children shouldn’t play in the fields in this heat, shouldn’t go to sleep without eating a meal and that there should be a massive awareness programme by the Bihar government to educate people,” Shah says.
“The government did a good job for those years, but this year, with resources being diverted to the Lok Sabha election, there has been a massive shortcoming in implementing the SOP,” he says.
Meanwhile, Jacob, his research partner on the paper, writes in The Hindu, “I don’t know what went wrong this year.”
Where was the awareness?
Back at SKMCH, a dozen parents say that their local ASHA or Anganwadi worker never visited their house at all.
Rohit Kumar had only heard of AES through the news.
“They were talking about litchis, that children are dying by eating them. That’s how we found out. No one from the government came to tell us anything,” he tells ThePrint.
Kumar earns Rs 300 a day in Muzaffarpur as a labourer. “I sweep the roads or help build them, depending on the work that comes my way,” he says.
On Tuesday, he owed his neighbour in Rs 500 for borrowing his car so he could take his son to the hospital, unaware that the government will reimburse him for the expense.
Neet Kumar, another man with a similar story, tells ThePrint that while he “knows there is an Anganwadi worker in his village, they never came to tell us anything”.
Even S.K. Shahi, the superintendent of the SKMCH says, “The awareness drives did happen, but perhaps not with the same magnitude. This slackness will not continue now, change will come.”
Sanjay Kumar, however, denies any government negligence.
“Our frontline workers were prepared, they distributed 7.5 lakh pamphlets with the Dos and Don’ts. Information has been given to the public through newspapers, through the radio and advertisements,” says the state’s principal health secretary.
Sinha vaguely remembers Kumar mentioning AES in a meeting as early as March. “He said he’s written a letter or something.”
An email outlining the course of standardised treatment as well as steps to prevent further spreading of this disease, was only sent out to hospitals, deans of medical colleges, district officials, health centres and the likes by the Bihar Health Society on 7 June.
The advisory, which came late into the rise in admitted patients, also did not consider the state of government-run healthcare in Muzaffarpur.
At SKMCH, up to six people are sharing one bed. Two nurses juggle a 100 people demanding their attention, and Dr Shashi Kumar Ravi, who first said he was an “intern”, can be found writing prescriptions in hyper-speed to a ceaseless stream of patients entering his office.
As of now, 12 extra doctors have been deputed to the hospital from surrounding districts to help ease the load.
Plans to increase hospital beds
Muzaffarpur is ill-equipped to deal with an outbreak of this magnitude — syringes litter the floor, children play next to piles of trash, and bedsheets soaked with urine go unchanged.
SKMCH, the largest and only medical college in the area, is functioning at 650 beds to every 900 people, Shahi tells ThePrint.
The chief minister, however, who met with protests outside the hospital Tuesday and has also had a PIL filed against him, promised to increase that number to over a 2,500.
The Bihar government is on the back-foot again, having to change its stance from prevention to cure in what appears to be a losing fight against AES.
The PIL against Nitish, Harsh Vardhan, and Bihar health minister Mangal Pandey is scheduled to be heard on 26 June.
Also read: Modi govt wants to define e-prescription format to regulate online sale of medicines
This report has been updated to correct the name of SKMCH superintendent.




The author, being an English literature graduate, might satisfy the criteria of good writing but absolutely fails in getting her facts right
One very important correction here. Blaming Harshvardhan is actually idiotic on the part of the media and the author. Yes, Harshavardhan was health minister in 2014 but he was there for barely 8 months when he was shunted out and replaced with J.P.NADDA. In the 4 years that J.P.NADDA was central health minister, he was the most useless as well as silent minister. He did nothing to improve health budget, nor improve health facilities, did not execute the promises of his predecessor, was only interested in WHO & UNICEF project deadlines, was more focussed on AYUSH rather than modern research and medicine and antagonised the whole medical workforce with a harebrained bill called NMC which is going to worsen the problems rather than solving them.
During his tenure, private & government medical colleges who have failed MCI inspections, were given permissions. Atleast 24 of them [my personal count according to various media reports that I have been tracking] were given such permissions and now after years of completing the MBBS courses, the colleges having repeatedly failed MCI inspections for 5 consecutive years have not gained recognition. A prime example is Fathima Medical College in Cudappah, AP. Now, all the college students have been ordered by the Central health ministry & supreme court to rewrite the entrance exams and redo the whole 5 year course.
I think the authors of your article should also focus on the history and wider picture to know what truly happened and then point the blame. Blaming people who had nothing to do with the expectations only results in discouraging them and failure to identify the culprit.
One hopes a lasting solution can be found by either 2019, the 150th anniversary of Mahatma Gandhi’s birth, or 2022, the 75th anniversary of India’s independence. Like the doubling of farmers’ incomes, that is what these promises with a five year horizon tend to deliver.