One cannot treat what one cannot detect. When we examine India’s diagnostic ecosystem, it is evident that it is overstretched. Today, there is only one radiologist for every 100,000 citizens in India, compared to far higher ratios in Europe and Singapore. This shortage forces India’s radiologists to interpret 100+ scans daily, increasing the likelihood of fatigue-related errors. Diagnostic equipment is also inadequate; with only 4,500 MRI machines, India has about a third of what is needed.
Poor detection capacity partly explains India’s dubious reputation as the global hub for tuberculosis, accounting for a quarter of the total cases. Additionally, India’s health needs are evolving rapidly, driven by a surge in lifestyle diseases and new infectious diseases. In short, India’s diagnostics ecosystem urgently needs a proverbial shot in the arm.
Within this milieu of challenges, an old yet new solution holds promise — technology. The rudimentary pre-modern approach to diagnostics, which relied mainly on visual inspection and patient descriptions, gradually evolved into the use of increasingly sophisticated tools. Early instruments like thermometers and stethoscopes gave way to advanced technologies such as microscopy, X-rays, CT scans, MRIs, and ultrasound. Today, technology can again help overcome new diagnostic barriers, not necessarily through new tools but by leveraging Artificial Intelligence (AI).
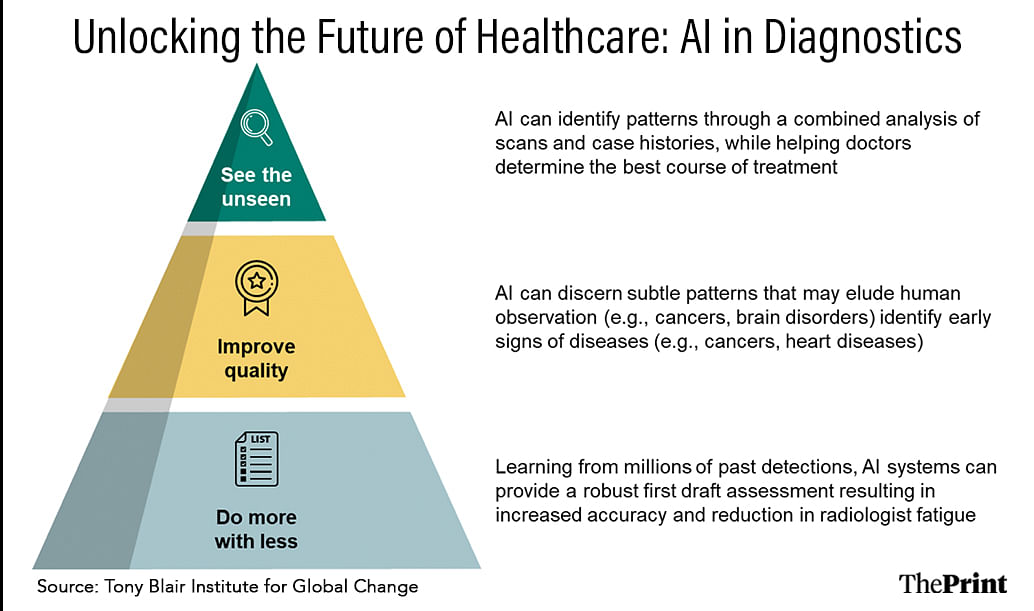
First, at a basic level, AI offers the opportunity to do more with less, i.e., enhance efficiency. AI systems can provide a robust first draft assessment by learning from millions of past detections. Studies show that AI models can differentiate between normal and abnormal chest X-rays with an accuracy of 99.1 per cent, which translates to a 58 per cent reduction in radiologist burden. A similar study by NHS (UK) found that AI can help save up to 2 hours per day for senior radiologists — allowing them to focus on more complex cases.
Second, AI can discern subtle patterns that may elude human observation. NIH found that AI models selected the correct diagnosis more often than physicians in closed-book settings, i.e., without referring to external materials such as online resources. Further, AI has been used to detect signs of breast cancer missed by doctors, and brain disorders, and identify early signs of several diseases, including various cancers, and cardiovascular illnesses.
Finally, and somewhat controversially, AI can help see the unseen — identify patterns that don’t exist on scans. Combining patient’s comprehensive case histories with scans can lead to impressive results, such as in Japan, where AI predicted diabetes onset from routine health check-ups with a 95 per cent accuracy. Moreover, advanced pilots are deploying AI to help doctors determine the most effective drug combination for treating lung cancer nodules.
Also read: DY Chandrachud is right about using tech in courts. Learn from Germany’s IBM AI assistant
Acknowledge risks
The integration of AI in diagnostics also presents risks. Unlike human errors, mistakes made by AI systems can affect thousands of patients simultaneously from a single algorithmic flaw. Moreover, AI’s reliance on large datasets raises issues of privacy and data security, as well as the risk of bias if the data used to train these systems is not representative of diverse populations. The lack of transparency in AI decision-making, often called the “black box” problem, makes it challenging to understand or trust the rationale behind AI-driven diagnoses. Despite these risks, with proper oversight, regulation, and collaboration between technologists and healthcare professionals, AI can be developed and deployed to mitigate its risks while enhancing its benefits.
AI can bridge India’s diagnostic gaps by enhancing efficiencies, improving quality, and predicting disease onset early. More importantly, it can bring high-quality care to rural and remote areas, bypassing the need for local personnel and infrastructure development. Recognizing this potential, the Indian government has initiated several digital health projects to lay the foundations for new AI systems. In 2021, a hospital in Tezpur, Assam, could easily install and use Qure.ai and provide radiology services to rural residents through remote support from a Mumbai-based hospital.
For India, the goal should be to integrate AI as a core component of a revitalised healthcare system, not just in isolated applications. This requires each state to adopt a comprehensive strategy for AI integration, including financial, administrative, technological, training, and legislative support. States should also establish dedicated units to foster strategic partnerships with health-tech companies, learn from global best practices, and build capacity among healthcare professionals. These units should oversee AI deployment and ensure continuous monitoring and evaluation to adapt and optimize these technologies. Strengthening the foundations of India’s healthcare system with AI could provide a robust platform to realize the nation’s development goals.
The author heads the India practice for the Tony Blair Institute for Global Change. Views are personal.
This article is part of a series on AI tech policy and impact as part of ThePrint-Tony Blair Institute for Global Change editorial collaboration.
(Edited by Humra Laeeq)