New Delhi: Scientists across the world have been working round-the-clock to gather new insights into the SARS-CoV-2 virus and how it affects humans, even as Covid-19 continues to claim lives. So far, over 9,33,343 people have died and more than 2.9 crore infected globally.
Here are some of the recent scientific studies on Covid-19.
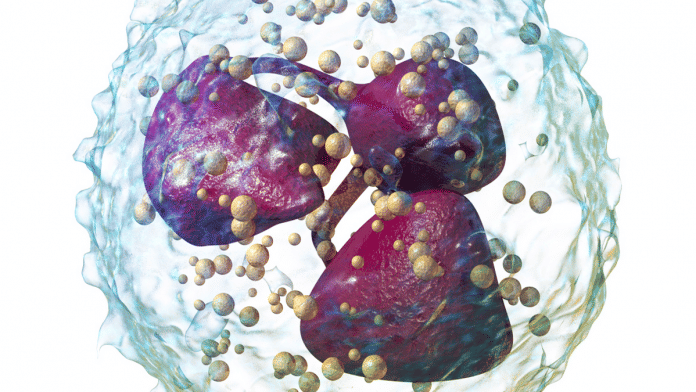
Webs of ‘sticky DNA’ behind tissue damage in Covid-19 patients
Much of the tissue damage that is linked to severe Covid-19 infection may be due to some sticky webs of DNA that are released from immune cells and known as neutrophils, scientists have said.
Two independent groups in Belgium and Brazil have published their work in the Journal of Experimental Medicine (JEM). The studies have suggested that blocking the release of these DNA webs could be a new therapeutic way to manage severe forms of Covid-19 infection.
Some Covid-19 patients experience an inflammatory response that can damage the lungs and cause acute respiratory distress syndrome (ARDS), leading to low blood oxygen levels and potential death.
An early indicator of severe Covid-19 is increased number of neutrophils, a type of white blood cell. Neutrophils catch and kill invading microbes by unwinding their DNA and forcing it out from the cell to form sticky webs known as neutrophil extracellular traps (NETs).
NETs can damage surrounding tissue, and can, therefore, cause some of the lung pathology associated with severe Covid-19.
Researchers have found large numbers of NETs dispersed throughout the lungs of patients who had succumbed to Covid-19. They were found in the airway compartment, where they almost completely obstructed the small bronchioles and alveoli that mediate gas exchange in bodies.
NETs were also found to have formed in the blood vessels near tiny blood clots, which are a common pathological feature of severe Covid-19 patients.
Also read: Scientists have taken the world’s biggest photo ever, and it’s of a cauliflower
Proteins from intestinal bacteria may reduce inflammation
Proteins from an intestinal bacteria known as bifidobacterium can help stop excessive or uncontrollable inflammation in Covid-19 patients, a study has found.
The study, published in the Anaerobe journal, suggests that a fragment of this protein can be used as an anti-inflammatory medication to manage coronavirus infection.
On encountering infectious pathogens, the cells of our body send out a signal to trigger an immune response. This signal is transmitted by proteins known as anti-inflammatory cytokines. Sometimes, this signalling goes into an overdrive, causing what is known as a cytokine storm — often observed in severe cases of Covid-19.
Some bacteria know how to trick our body’s protective systems by capturing cytokines and reducing inflammation.
The new study demonstrates the mechanism used by bifidobacterium to create this anti-inflammatory process.
The researchers conducted an experiment to study how FN3, a surface protein of bifidobacterium, blocks or binds cytokines. The team has suggested that this surface protein can reduce the levels of cytokine storm in Covid-19 patients.
Tiny antibody component for a potential Covid-19 drug
Scientists have isolated the smallest biological molecule that neutralises the SARS-CoV-2 virus and used it to construct a potential drug against Covid-19.
The component is 10 times smaller than a full-sized antibody. It has been used to construct a medicine dubbed Ab8. According to the study, published in the journal Cell, this drug has been highly effective in preventing and treating SARS-CoV-2 infection in mice and hamsters.
The tiny antibody has many advantages. It increases its potential for diffusion in tissues to better neutralise the virus. It also makes it possible to administer the drug by alternative routes, including inhalation, researchers have said.
The antibody does not bind to human cells, which, the team says, is a good sign because it won’t have negative side-effects in people.
Substance use disorder linked to higher Covid-19 risk
People with substance use disorders are more susceptible to Covid-19 and its complications, a new study has found.
The research, published in the journal Molecular Psychiatry, suggests that healthcare providers should closely monitor patients with substance use disorders and develop action plans to help protect them from infection and severe outcomes.
Health records from the US shows that 10.3 per cent of its population who suffered from substance use disorders represented 15.6 per cent of the total Covid-19 cases, noted the study.
The analysis revealed that those with recent substance use disorder diagnosis were more likely to develop Covid-19. The susceptibility was strongest for opioid use disorder, followed by tobacco use.
People with such disorders are also more likely to experience worse Covid-19 outcomes such as hospitalisation and death than those who did not suffer from them.
Researchers have also said that this disparity may be explained by the fact that the lungs and cardiovascular system are often compromised in people who suffer from substance use.
Immune suppressing drugs do not increase Covid-19 risk
Patients on immunosuppressive therapy for common skin and rheumatic diseases are not at increased risk of contracting Covid-19, according to scientists who said people should continue to take their medicines as prescribed.
Diseases like psoriasis and rheumatoid arthritis are a result of an overactive immune system. These patients are usually prescribed medications that suppress the immune system activity.
There was some concern that such patients may be at increased risk of Covid-19 due to their weakened immune system. However, a study published in the Journal of the American Academy of Dermatology shows that these people are not at any greater risk of Covid-19 than the general population.
The team conducted an analysis of 213 patients who were taking immunosuppressive medication. Thirty-six per cent of them tested positive for Covid-19, and had no greater odds of being hospitalised or placed on a ventilator than the general population.
There was no evidence that any single immunosuppressive medication increased a patient’s odds for testing positive or developing a serious infection.
Also read: Covaxin produced ‘robust’ immune response in monkeys, ICMR paper says