New Delhi: When the Pradhan Mantri Jan Arogya Yojana (PMJAY) was launched in 2018, its purpose was to save households from being impoverished as a result of catastrophic medical expenditure. However, data with the National Health Authority (NHA), which manages the scheme, shows that the second-most-claimed procedure under the tertiary healthcare programme is the Covid screening test.
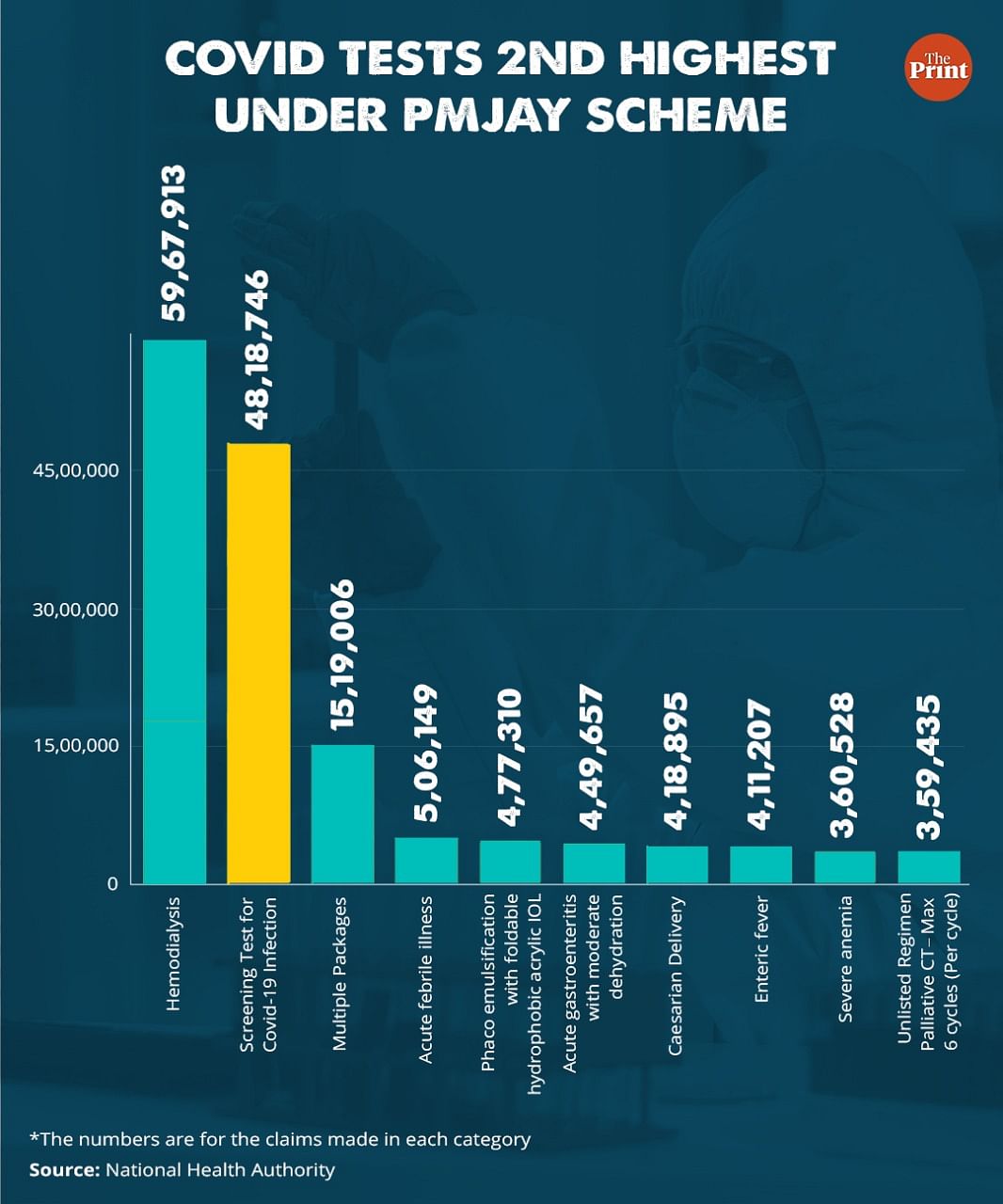
NHA data (updated till 8 August, 2022) shows that with 48,18,746 claims, Covid screening tests are second only to hemodialysis (59,67,913 claims) in the top procedures that have been funded under PMJAY. The total money sanctioned for these tests stands at Rs 441,41,22,350 (the average cost per test comes to a little over Rs 900).
Covid screening tests — both rapid antigen tests and RT-PCR — can now be accessed for a few hundred rupees, although officials say they were included in PMJAY earlier on when they were more expensive. Moreover, the tests neither qualify as treatment, nor do they require hospitalisation.
Meanwhile, the greatest number of claims made under PMJAY have been for hemodialysis, even though the government has had a dedicated National Dialysis Programme to ease access to the treatment since 2016.
ThePrint reached NHA CEO R.S. Sharma over the phone and WhatsApp, and the Union health ministry over email, but had received no response when this report was published. The article will be updated when a response is received.
Also read: 11% of 69 crore eligible people have taken Covid precaution dose, says govt, blames waning fear
Why Covid tests became part of PMJAY
PMJAY is the tertiary care arm of the NDA government’s flagship health programme Ayushman Bharat, and provides annual health cover of Rs 5 lakh per eligible family.
In a statement issued on the day of the scheme’s launch in 2018, the Press Information Bureau had said: “Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (PMJAY) will provide a cover of up to Rs. 5 lakhs per family per year, for secondary and tertiary care hospitalisation…The objectives of the yojana are to reduce out-of-pocket hospitalisation expenses, fulfill unmet needs and improve access of identified families to quality inpatient care and daycare surgeries.”
Government sources said that when Covid screening tests were first introduced in the list of packages for which PMJAY would provide coverage, the tests were much more expensive, running into a few thousands.
“When they were introduced into the list, the tests cost something like Rs 4,500. At that point it made sense, because it was not something the PMJAY target population could afford, and there was a need to do the tests when required to prevent the spread of the disease,” said an NHA old-timer, who chose to remain anonymous.
The old-timer added: “But the cost of the test has come down drastically. It should have been removed long back, because it now costs as little as Rs 150. It is a drain on resources. To have continued with it under PMJAY is a scandal, especially when the prime minister himself has said on multiple occasions that the purpose of the scheme is to reduce catastrophic health expenditure”.
A senior NHA official, however, tried to play down the numbers by saying that the numbers were “mostly from 2020-21″, when the pandemic was at its peak.
“When Covid happened a decision was taken on compassionate grounds to make the test accessible for the larger population. I do not think too many Covid test claims were made in the last year or so. We do not fund anything other than secondary and tertiary care,” the official said.
Programmatic overlap?
The procedure for which most claims have been made under PMJAY is hemodialysis. This, despite the fact that since 2016, the government of India has also been running a National Dialysis Programme to ease access to the procedure. Hemodialysis is is expensive, and once started in a patient, cannot be discontinued.
NHA sources say there are at least 12 national programmes — including for cataract surgeries and normal deliveries — that are also covered under PMJAY, but a decision to trim them out of the PMJAY list was never actioned, leaving the door open for possible misuse.
“These should have been trimmed out because only then can the funds allocated for PMJAY be used for the purpose for which they are meant. However, there is a strong resistance to change,” said a person formerly associated with the scheme.
The senior NHA official quoted above said that the dialysis programme under the National Health Mission does not support dialysis in the private sector.
“We decided to include dialysis as an additional support system for our beneficiaries, many of whom live in rural areas where access to dialysis facilities is limited,” the official said.
(Edited by Poulomi Banerjee)
Also read: 18,606 fraudulent hospital transactions found in Ayushman Bharat insurance scheme, govt tells RS



