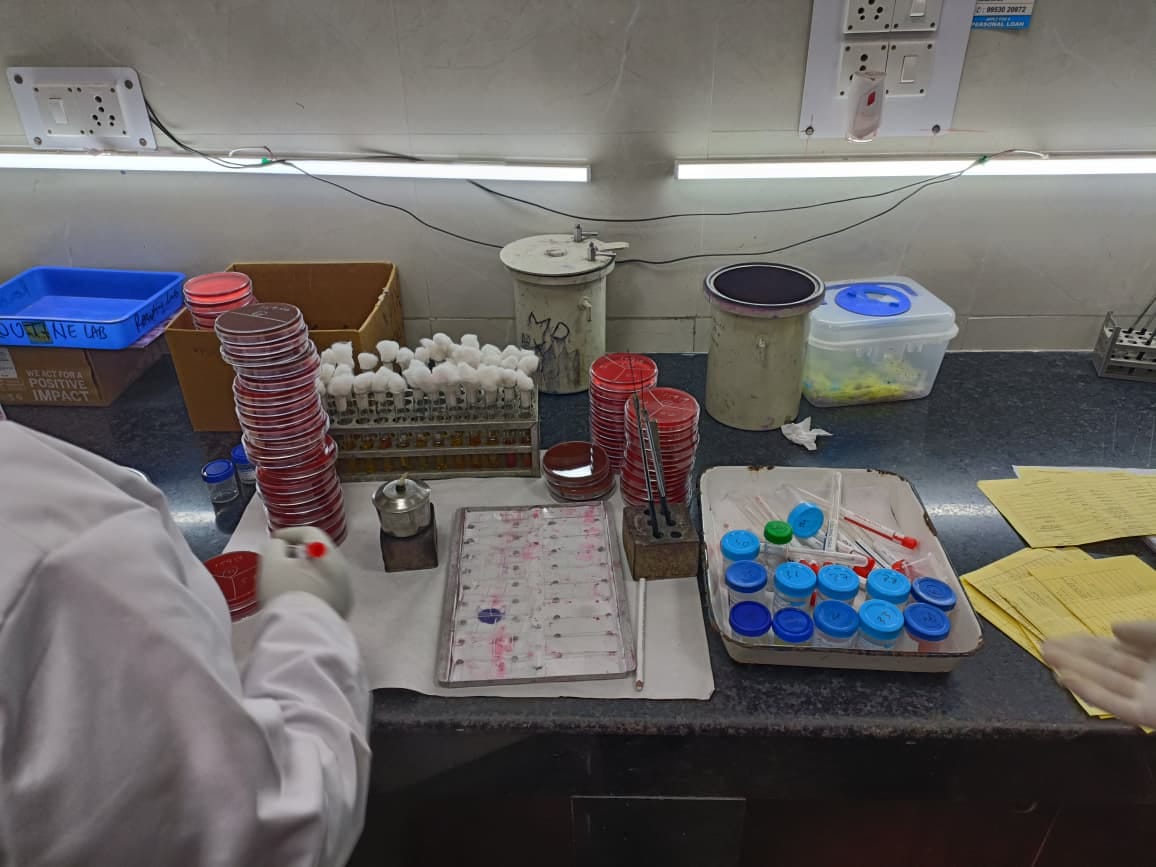
New Delhi: A tray carrying a pile of urine samples is wheeled into the routine bacteriology lab at the Lady Hardinge Medical College in central Delhi. It is liquid gold for researchers in the microbiology department—they’re on the frontlines of India’s battle against drug-resistant bacteria, and these are their weapons.
The century-old Lady Hardinge Medical College and Hospital in Delhi is part of India’s National Antimicrobial Resistance Surveillance Network (NARS-Net). Along with 54 other hospitals across the country, LHMC’s microbiology lab routinely tracks, identifies, and studies the different disease-causing bacteria and how they are becoming resistant to antibiotics.
“Antimicrobial Resistance or AMR is one of the biggest threats in India right now,” said Manoj Jais, Director of the Department of Microbiology. “Imagine so many bacteria that cause curable diseases like pneumonia and UTIs just stop responding to antibiotics. It needs to be studied and addressed,” he added.
India is the biggest consumer of antibiotics globally and drug-resistant bacteria presents a grave challenge. In 2025, the World Health Organization flagged AMR as one of the top 10 global health threats, and especially pointed to India, saying its “resistance rates were among the highest in the world.” Overuse and misuse of antibiotics, self-medication, and antibiotic exposure through environmental factors like agriculture and poultry are the main reasons for high rates of AMR globally, according to the WHO.
India began its National Programme on AMR Containment in 2013, to survey, study and understand antibiotic resistance in different bacteria in the country. This is where the Lady Hardinge Medical College comes in.

LHMC’s microbiology lab, as part of the national network, is tasked with “determining the magnitude and trends” of AMR in its region. As a tertiary care hospital, they treat over a thousand patients every day, with a spectrum of bacterial, fungal and viral infections. The microbiology lab receives 200-300 samples daily of urine, blood, and pus, as well as respiratory swabs from inpatient departments and ICUs.
The samples are processed, and the bacteria causing the diseases are identified. Then, the researchers test each bacterium’s resistance to existing antibiotics, noting down the level of resistance towards each drug. This information, compiled monthly, is fed into the National Centre for Disease Control (NCDC)’s database. It also helps in treating the patients in the hospital with the correct, most effective antibiotics.
“Our work helps our patients and doctors daily, by identifying and treating drug-resistant bacterial infections,” said Dr Jais. “At the same time, we’re helping the country do it too.”

Also read: Dementia wave is hitting Indian homes. Families are exhausted, healthcare unprepared
How AMR surveillance is done
LHMC was one of the first hospitals to join the NARS-Net when it was established as a pilot project back in 2017. For nine years now, they’ve been feeding data to India’s global network. It has helped establish which bacteria are the most resistant to drugs, which samples the bacteria commonly originate in, and which drugs show increased inefficacy in which parts of the country. Along with collecting samples and data, the doctors have also developed an understanding of how prevalent AMR is in the community.
Inside the first-floor lab of the microbiology department, researchers and technicians are busy labelling the day’s samples. Samples, chosen by the doctors attending to patients, are sent to the microbiology department, which then isolates the bacteria, cultures it and studies it to understand its antibiotic resistance. The entire process takes a day or two.
While stacking agar plates to be stored inside the hot room to help grow the bacteria, Dr. Jais explained how he uses a simple example to help patients understand AMR. Comparing bacteria to people, he explains how, after multiple uses, the bacterium familiarises itself with the antibiotic and stops responding to its treatment.
“If you meet me multiple times, you’ll recognise me. Same way, the bacteria recognise an antibiotic, and then evolve to counter it,” said Dr Jais. “For the first few times, an antibiotic can be effective against bacteria. But over time, the bacteria develop a resistance, and the antibiotic then becomes useless.”
Dr Sanjib Gogoi, an associate professor in the microbiology department, said patients with common colds and infections are spending weeks in the hospital because the bacteria causing the infection is resistant to most antibiotics. A large reason, he said, is self-medication.
A 2021 study by the University of Washington found that over 3,00,000 lives have been lost every year in India since 1991 due to antimicrobial resistance. For Dr Gogoi and Dr Jais, these are not just statistics, they’ve seen these deaths.
“Even before patients come to see us with illnesses, they start self-prescribing and taking over-the-counter antibiotics,” said Gogoi. “Without proper identification of the bacteria and the required drug for it, patients don’t realise they’re only endangering their own lives by taking medicines themselves,” he added.
The annual NARS-Net report from 2024, which collated information from all 54 hospital sites, including LHMC, shows that the most common bacterial pathogens are E coli and Klebsiella. They are associated with urinary tract infections and pneumonia, but when they become drug-resistant, even these diseases are life-threatening.

LHMC doctors concur with the findings of global studies on AMR, noticing trends of increasing multidrug resistance—when a bacterium is resistant to more than three classes of antibiotics—especially bacteria found in ICUs. According to Dr Shweta Satija, an associate professor in the microbiology department, they are also increasingly seeing cases of bacteria that are resistant to colistin, which is a strong antibiotic only used in the most severe cases.
“Colistin is our last case scenario; we give it when no other drug works. If there are bacteria resistant to colistin too, what can we do next?” she asked.
Also read: Cough syrup deaths—how contaminated Coldrif slipped past regulators
An AMR pandemic
The latest AMR 2.0 National Action plan was released on 18 November by the Union Ministry of Health and Family Welfare. During its release, Union Minister JP Nadda called antimicrobial resistance a ‘pandemic’ that is impacting several developing countries.
The government’s new plan expands AMR monitoring to private sector hospitals, and even talks about integrating human, animal, agriculture and environment sectors to better manage antibiotic use and resistance in the country.
“The unregulated use of antibiotics in poultry may have serious implications for developing economies, especially for India,” said Gajender Kumar Sharma, India country director of non-profit organisation, World Animal Protection, in a press release. “There is ample literature linking the indiscriminate use of antibiotics with the rapid development of Antimicrobial Resistance (AMR) in various livestock sectors, including poultry and aquaculture in India,” he added.

Given the huge and immediate challenge of AMR in healthcare, LHMC has its work cut out for it. In a country with more private hospitals than public, the concerns of overuse of antibiotics are even higher outside the LHMC’s purview.
“In a day and age where antibiotics are so over-prescribed that even pharmacies hand them out regularly without a prescription, how do you build awareness about AMR in people?” asked Dr. Gogoi. “We’re doing our best for our patients, but there definitely needs to be an overhaul in the way people see AMR.”
(Edited by Theres Sudeep)







This is a global threat and in countries like India where people are just not aware about how abusing anti microbial drugs can lead to this threat of drug resistant bacteria which only makes the society more vulnerable.
As the economy grows, more people will become dependent on such medicines. Generally I don’t promote “alternative treatments” but for simple cough or fever, please stick to Ayurveda.
Btw I have no issues with alternative treatments like Ayurveda but it cannot be the lone option for treating serious illnesses. Ayurveda is a better lifestyle choice than a treatment option.