New Delhi: In an accidental find, chemistry researchers at the University of Warwick in England have discovered a new, extremely potent antibiotic that can kill seven different types of bacteria, including those causing skin, blood and urinary infections.
The antibiotic was discovered during the process of making another, more common antibiotic, methylenomycin A which is effective against most gram-negative bacteria, but not against drug resistant bacteria types. The discovery of this new antibiotic is highly significant given how antimicrobial resistance (AMR) is on the rise.
The new antibiotic, premethylenomycin C lactone, is 100 times more potent than methylenomycin A, even though it is technically an intermediate compound and is produced naturally by the same bacteria that make methylenomycin A.
“As humans, we anticipate that evolution perfects the end product, and so you’d expect the final molecule to be the best antibiotic, and the intermediates to be less potent,” Gregory Challis, a chemistry professor at the University of Warwick and one of the authors of the study, said in a press release.
When Challis and his team began isolating enzymes and found intermediate products like premethylenomycin C lactone, they found that it had antibacterial activity too. When tested, the scientists found that only 1 microgram of premethylenomycin C lactone was enough to kill 1 millilitre of the bacteria S aureus, which causes skin, blood and internal infections. Meanwhile, about 256 mg of Methylenomycin A was needed for the same use.
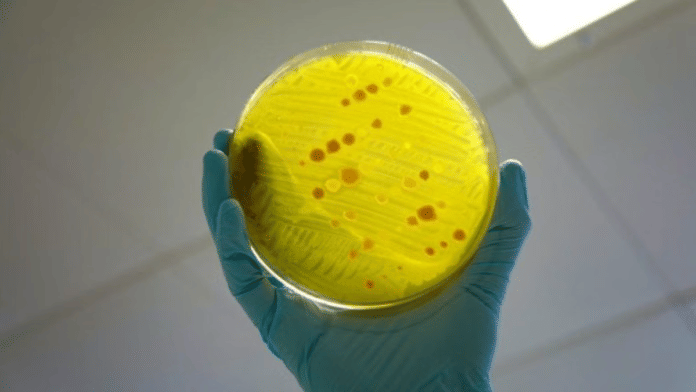
Published in the Journal of the American Chemical Society on 27 October, the paper describes how the scientists decided to isolate and study each enzyme in the bacteria that makes methylenomycin A. Named Streptomyces coelicolor A, the bacterium is found in soil and has for years been a common origin for several antibiotics.
Antibiotics are normally formed by various bacteria for their personal defence mechanism, since certain fungi and other bacteria might threaten their food and livelihood. These antibiotics are then harvested and used by humans to help the immune system survive bacterial infections. However, the process of making antibiotics in bacteria goes through many chemical reactions, and at each stage, new compounds are formed.
“Methylenomycin A was originally discovered 50 years ago, and while it has been synthesised several times, no one appears to have tested the synthetic intermediates for antimicrobial activity!” said Challis.
Also Read: 1st US FDA-approved drug invented in India set for local launch as part of combination antibiotic
Why it’s important
According to a Nature article, antimicrobial resistance (AMR) could cause more than 39 million deaths over the next 25 years. AMR essentially means that certain disease-causing bacteria, microbes and viruses have developed a resistance to the drugs that were initially used to stop them.
One of the ways to tackle antimicrobial resistance is to develop newer, stronger and more innovative antibiotics, said the Nature article. However, the antibiotics industry is suffering from ‘too few drugs in the pipeline’, according to a report by the World Health Organization published on 2 October.
“The pipeline faces a dual crisis: scarcity and lack of innovation. Among the 90 antibacterials in development, only 15 qualify as innovative,” read the WHO report.
Given the grave risk of AMR for health globally, the new study and discovery by the University of Warwick researchers signals good news for the antibiotic research pipeline, and for combating antimicrobial resistance.
(Edited by Ajeet Tiwari)
Also Read: What is antibiotic resistance and how we can tackle it