Have you ever had a rash after being exposed to sunlight? If yes, there’s a high chance that you might have a sun allergy known as photodermatosis. In India, where we have abundant sunlight on most days of the year, understanding this condition is paramount. People with photodermatosis experience an array of symptoms, ranging from rashes and redness to blisters and itching after staying outdoors.
Photosensitivity arises from an atypical response to a specific segment of sunlight’s electromagnetic spectrum and the presence of a skin-based chromophore, a reactive compound. Sensitivity might be due to a particular spectrum of sunlight such as ultraviolet A or B (UVA, UVB) or extend to visible light or a broader electromagnetic spectrum. UVA sensitivity stands out as the prevailing form. Additionally, it’s crucial to acknowledge that certain individuals possess a genetic predisposition to photodermatosis. Environmental catalysts for photodermatosis encompass sunlight, medications, chemicals, and underlying medical conditions.
There are two types of photodermatitis, broadly classified as endogenous and exogenous photodermatosis.
Endogenous photodermatosis is caused by autoimmunity responses. The condition encompasses polymorphic light eruption (PMLE), actinic prurigo, hydroa vacciniforme, solar urticaria, and chronic actinic dermatitis. Exogenous photodermatosis is triggered by some foreign substance. It is classified into phototoxic and photoallergic dermatitis and is usually drug-induced (tetracyclines, fluoroquinolone, NSAIDS, oral retinoids, dapsone, griseofulvin, quinidine, hydrachlorothiazide, statins). Phototoxic dermatitis resembles a sunburn that has a rapid onset, which can vary between minutes and hours. It occurs when a person is exposed to a sufficient amount of light and a photosensitive drug for sufficient sufficient to cause a reaction. The resultant rash is localised to the area of exposure. Photoallergic dermatitis, though, is rarer compared to phototoxic reactions and is dependent on prior exposure to allergens, either systemically or topically. The onset of this condition is delayed — it starts between 24 and 72 hours.
Also read: Don’t go holidaying to a beach if you have psoriasis. There’s a trick to…
The diagnosis process
Photodermatosis diagnosis involves a comprehensive evaluation of skin lesions resulting from sunlight exposure. Identifying the specific type of photodermatosis entails a thorough study of medical history, skin examination, and specialised tests. This includes the following tests.
Minimal erythema dose (MED) testing: Conducted with broadband or monochromators, it determines the threshold dose of radiation required to induce skin redness.
Provocation phototest: This process exposes the patient’s skin to increasing doses of UVA and UVB light over four consecutive days to replicate the dermatosis.
Photopatch tests: Performed in conjunction with standard patch tests, these tests assess for photoallergy. Two sets of photoallergens are applied, with one set being irradiated (exposed to radiation) and the other serving as a control.
In addition to these tests, a dermatologist might recommend a skin biopsy and other laboratory investigations.
It is essential to consult a qualified dermatologist who can provide the right guidance and treatment options tailored to your specific skin condition.
Treatment for photodermatosis is not a one-size-fits-all solution, especially in a country as climactically and demographically diverse as India. Dermatologists offer tailored solutions, including topical creams, antihistamines, and phototherapy. For Indian skin, it’s crucial to consult a dermatologist who understands the intricacies of our skin tones.
Also read: Do you think toners can shrink pore size? You’re wrong
Prevention comes first
Prevention isn’t just a strategy — it can be your shield against photodermatosis.
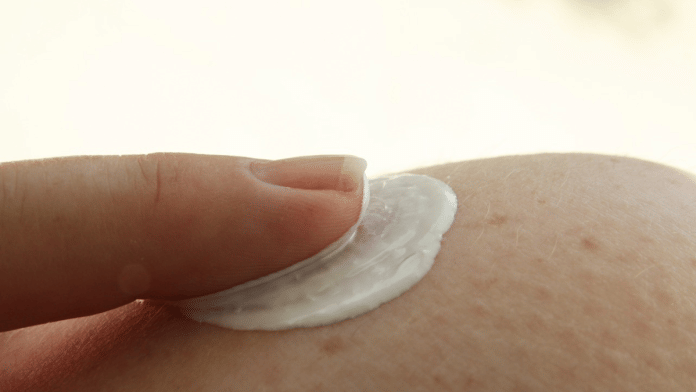
Sunscreen is the silent guardian for most skin problems. It is crucial to use a broad-spectrum sunscreen with an SPF of 50 or higher and cover all exposed skin. Make sure that the sunscreen offers protection against both UVB and UVA rays and is water-resistant too. Apply it generously and reapply every two hours when outdoors. Remember that makeup with an SPF is insufficient for adequate protection. Additionally, you must apply your sunscreen even when you’re indoors and on cloudy days.
Covering vulnerable areas and wearing a wide-brimmed hat can help those who suffer from photodermatitis. Today, you can even get clothes with an ultraviolet protection factor (UPF). Thick, tightly woven, dry, and dark-coloured polyester, denim, and wool offer the best protection.
Time your outdoor activities. Plan them either before 10 am or after 4 pm. If you must be outdoors during peak hours, seek shade whenever possible.
Tanning products with dihydroxyacetone are photoprotective against UVA primarily and, to a lesser extent, against UVB.
You can also boost your intake of Vitamin D and antioxidants through supplements, wear a mask to protect your face, and use grey-tinted laminated glass for your vehicle’s windows and photoprotective UV films at home. Avoid consuming limes, parsley, celery, and wild parsnip, which can trigger photodermatosis. Moreover, get regular check-ups done to screen for skin cancers.
Photodermatosis isn’t curable, but it can be managed well provided you follow your dermatologist’s instructions. Most importantly, taking good care of your health can help much more than medicines. To that end, focus on your diet and precautions and avoid looking up quick fixes on the internet.
The author holds an MD in dermatology, venereology, and leprosy. She is currently working as a specialist dermatologist in ESIC, Okhla, New Delhi. Views are personal.
(Edited by Humra Laeeq)