The World Health Organization’s detailed note on the unprecedented outbreak of mpox, formerly called monkeypox, in the Democratic Republic of the Congo, has called for urgent intervention. The outbreak has already resulted in 7,851 reported cases and 384 deaths until May this year, with a case fatality rate of 4.9 per cent.
Infectious diseases transcend national borders, making it essential for countries to work together to combat outbreaks. The spread of mpox in Congo highlights the critical and urgent need for global collaboration and data sharing.
Public health experts fear the number of cases could be significantly higher due to limited testing and disease confirmation, worsened by the ongoing humanitarian crisis in the country. The outbreak was initially reported by the government in September 2023 and has since spread through various means including sexual and non-sexual physical contact as well as healthcare settings. Alarmingly, children account for over 62 per cent of the fatalities despite comprising only about 39 per cent of the total cases.
This outbreak adds to the challenges faced by Congo, which has been grappling with armed conflicts, widespread violence, and egregious human rights violations. The country also faces acute food insecurity worsened by frequent floods, epidemics, and large-scale displacement of populations, which further strains the already burdened healthcare system and severely challenges international aid efforts.
According to the United Nations High Commissioner for Refugees (UNHCR), over 6.2 million people have been internally displaced in Congo, while more than a million have sought refuge in neighbouring countries.
Denmark lab, Madrid saunas
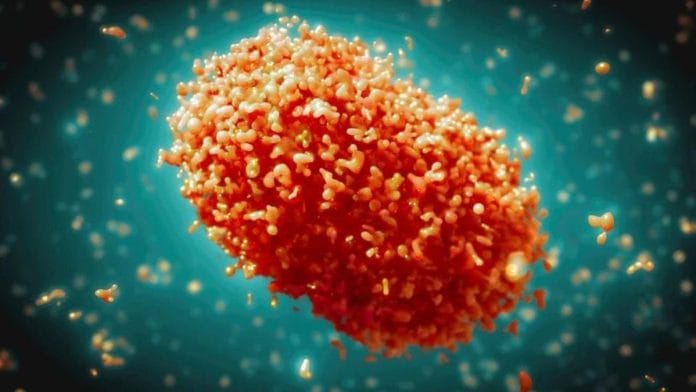
The mpox virus was initially identified in Denmark during a 1958 laboratory outbreak among monkeys. It wasn’t until 1970 that the first cases were reported in humans. Since then, sporadic outbreaks of animal-to-human and human-to-human transmission have occurred predominantly in Central and West Africa, often resulting in significant mortality.
Close contact with animals near forested areas may have facilitated these spillover events. In Central Africa, these outbreaks have typically been self-limiting due to the need for close contact for transmission. While monkeys are incidental hosts, the actual reservoir remains unknown, though rodents and nonhuman primates are considered potential reservoirs.
The global awareness about monkeypox dramatically increased in early May 2022, when an outbreak stemming from an event in Madrid rapidly spread worldwide, primarily through sexual networks among men who have sex with men. This prompted the WHO to declare it a Public Health Emergency of International Concern (PHEIC), which remained in effect until 2023.
The 2022 outbreak continues to affect numerous regions worldwide, with the WHO estimating that it has afflicted over 97,000 people and led to more than 200 deaths in two years.
Also read: What $7 bn ‘minerals-for-infra’ pact with China could mean for Democratic Republic of Congo
Clades of mpox
Genome sequencing of pathogens has proven invaluable in understanding the origin, evolution, and genetic epidemiology of mpox outbreaks. Analysis of the mpox virus genomes from Africa and around the globe has revealed two distinct clades: the Congo Basin/Central African clade (Clade I) and the West African clade (Clade II).
Clade II, responsible for the global outbreak, is considered to have originated in Nigeria around 2017 before triggering the super-spreader event.
A 2024 early preprint describing the genome sequences from the recent outbreak in the town of Kamituga in Congo suggests that the genomes belong to a distinct sublineage of Clade I (Ib), dating its emergence to July-September 2023, which is consistent with local infection reports. Interestingly, the genomes had stretches of high similarity with those sequenced from previous zoonotic infections.
It is also noteworthy that this new viral lineage is characterised by a large genomic deletion of almost 1,000 bases. This deletion occurs in the part of the virus’s genetic material that is used by diagnostic tests such as PCR to detect its presence, making the tests less accurate.
Also read: Oropouche virus is rapidly spreading in South America. It can cause large outbreaks
Why should the world be worried?
The global community should be deeply concerned about this outbreak for several reasons. First, the transmission and case fatality is estimated to be significantly higher than what was observed in the 2022 global outbreak. Second, Congo’s dense population and widespread outbreaks, coupled with limited testing and resources due to ongoing crises, pose serious challenges.
The displacement of people further increases the risk of the infection spreading to neighbouring countries that are populous and have fragile healthcare systems, making them ill-prepared to contain an outbreak.
Also read: How Indians’ genomes can end up abroad & why it’s raising ethical, ‘national security’ questions
Countermeasures and vaccines
The smallpox/vaccinia vaccine provides cross-protection against mpox. Although the vaccine was discontinued globally in 1980 after smallpox was eradicated, many countries still maintain emergency stockpiles. After the 2023 mpox outbreak prompted renewed interest, multiple companies have begun producing the vaccine.
In a bid to address the unprecedented outbreak, Congo has approved the emergency use of two mpox vaccines: Jynneos by Bavarian Nordic and LC16 by KM Biologics. While these vaccines are readily available in the West following the large mpox outbreak in 2022, African nations don’t have access to vaccines and treatments. The lack of vaccines in Congo is exacerbated by logistical challenges, national and international regulatory obstacles, inadequate funding, and competing disease outbreaks.
Gavi, the vaccine alliance, is prepared to facilitate vaccine donations from the United States and Japan. However, purchases for lower-income countries await WHO prequalification, wherein the WHO assesses vaccines against international standards to ensure they are safe and effective before they can be distributed in these countries.
Sharing data, technical know-how, and resources including vaccines and personnel can help ensure a coordinated and effective response. In the fight against infectious diseases, no one in our hyper-connected world is safe—until everyone is.
Dr Bani Jolly is a senior scientist at Karkinos Healthcare. She tweets @bani_jolly. Dr Vinod Scaria is a senior consultant at Vishwanath Cancer Care Foundation and adjunct professor at IIT Kanpur and DY Patil Vidyapeeth. He tweets @vinodscaria. Views are personal.
(Edited by Prasanna Bachchhav)