Hong Kong: The latest surge in Covid-19 cases is widening one of the biggest inequities of the pandemic era: The gap between nations that have messenger RNA vaccines and those that don’t.
The cutting-edge technology, which made its debut during the pandemic, has proven more effective than any other in staving off infections and serious illness from the coronavirus. Yet just a handful of facilities in the U.S. and Western Europe account for almost all of the world’s mRNA vaccine supply — leaving many countries in a desperate race to catch up.
From South Korea to Indonesia and South Africa, governments are seeking to set up mRNA production and develop other collaborations in the space, but they’re also realizing it could take them years to master the new science, leaving their countries reliant on less potent vaccines that potentially expose them to repeated waves of Covid and delay their economies from re-opening.
In South Africa, where Covid shots are in such short supply they’ve only distributed enough to cover about 5% of the population, the government last month teamed up with the World Health Organization and local drug manufacturers on an ambitious plan to turn the country into a hub for the first Made-in-Africa mRNA vaccines.
One critical element was missing from the plan: A company that knows how to make mRNA vaccines. For the fastest access, the South African hub would need one of the three developers already producing mRNA Covid shots to transfer their knowhow, but so far Cambridge, Mass.-based Moderna Inc. hasn’t committed, and neither has New York-headquartered Pfizer Inc. or its German partner BioNTech SE.
“These are businesses, we know that it’s not very easy for them to make decisions,” Bartholomew Dicky Akanmori, the WHO’s regional advisor on vaccine regulation, quality and safety for Africa, said in an interview. “They are reluctant.”
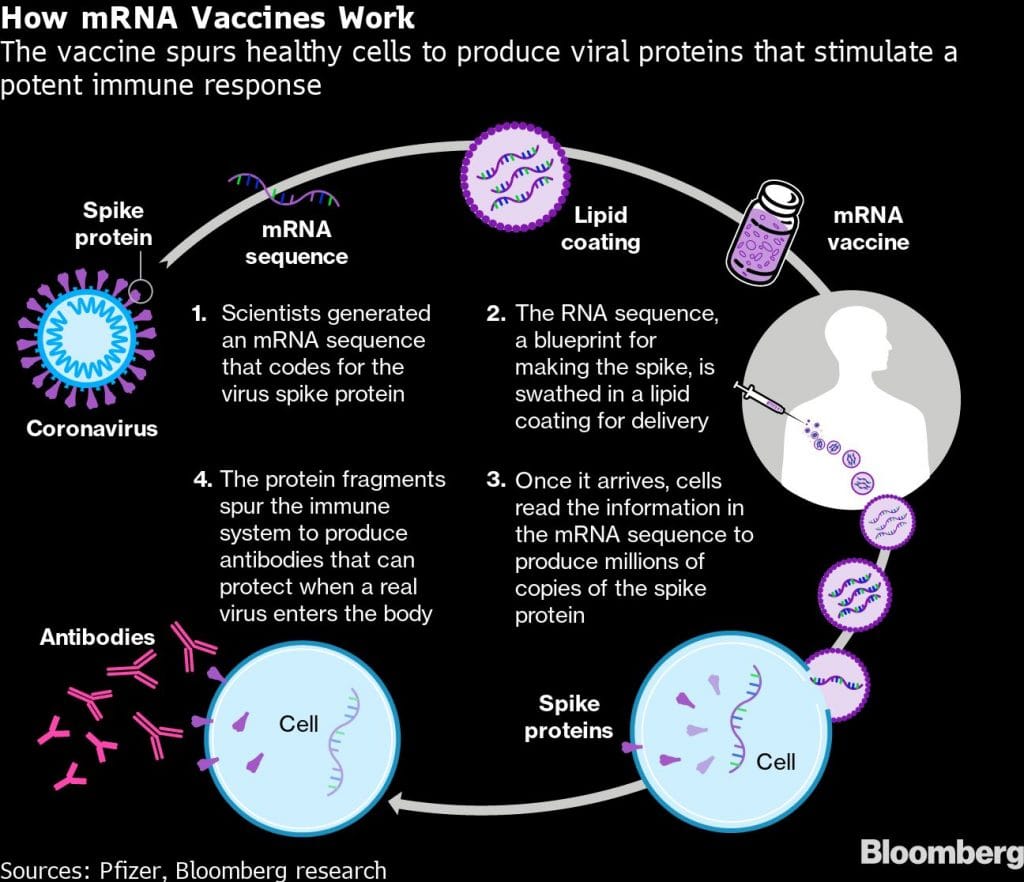
Without that kind of access, scientists in places like South Africa would need to perfect the tricky process of making an mRNA vaccine, which involves steps like the production of lipid nanoparticles, the vehicles used in an mRNA shot to deliver genetic code that helps trigger the body’s immune response.
They’d then have to then develop, test and mass-produce the vaccines, which could potentially take years and require resources that many nations, especially poorer ones, don’t have access to. With mRNA technology set to be used in everything from shots to combat other viruses to cancer drugs, that lack of infrastructure could put them on the pharmaceutical back-foot for years.
The mRNA supply gap is most obvious in Africa, where few people have access to them, said Hannah Wanjie Ryder, chief executive officer at Development Reimagined, a Beijing-based NGO focused on Africa and China. That’s left them reliant on vaccines which use older technology like those made by Sinopharm Group, Sinovac Biotech Ltd. or AstraZeneca Plc which largely protect against severe cases of Covid-19, but are less effective at stopping transmission and combating the contagious new variants that are emerging.
But it’s not just the poorest nations concerned about mRNA access. Achieving domestic production of mRNA shots has become a national security issue in some countries, given the supply-chain glitches, export curbs and demand spikes that have beset the wider Covid vaccine rollout.
“People in Korea say to the government why don’t we have such vaccines of our own?” said Sun Woo Hong, CEO of a new vaccine subsidiary of OliX Pharmaceuticals Inc., which is based near South Korea’s capital Seoul. “As a Korean, to have the mRNA vaccine development platform in Korea is very important.” The company last month agreed to collaborate on an mRNA vaccine with local conglomerate Samyang Holdings Corp. and on mRNA products for other diseases with GC Pharma.
Also read: It’s not Ivermectin but the human immune system that can fight Covid better
Need the tech
Malaysia’s state-backed Institute for Medical Research is in the early stages of developing several Covid vaccines, including one based on mRNA technology. Indonesia, currently in the grip of its worst Covid outbreak to date, is in talks with mRNA producers to transfer technology so local manufacturers can begin making the vaccines, Health Minister Budi Gunadi Sadikin said on July 2.
“We really want to invest in mRNA vaccines,” he said. “What we need is the access to the vaccine technology.”
So far, the big mRNA players haven’t embraced ambitious visions of global hubs or sharing their tech, though they are starting to make a bigger push overseas.
Pfizer, which makes its mRNA vaccines at several plants in the U.S., in May said it will make them in Ireland, and Croatia’s Prime Minister, Andrej Plenković, said Pfizer would make vaccine ingredients in his country, too.
Its partner BioNTech will start construction this year on a Singapore plant, its first factory in Asia, with production to begin in 2023. CEO Ugur Sahin said in April the company was also discussing the possibility of production in Africa.
Tying up with additional partners will be considered, but “this requires a diligent assessment as mRNA manufacturing necessitates GMP certified state-of-the-art manufacturing standards,” a BioNTech representative said. “If any of the predefined requirements are not met, the quality, safety and efficacy of the vaccine cannot be ensured – neither by the manufacturer nor the innovator.”
In May, Moderna announced a deal with Samsung Biologics Co. for the South Korean company to provide fill-finish services for its Covid vaccine and said it may seek production contracts or licensing agreements in Japan. Moderna has discussions underway about potentially expanding its manufacturing supply, said Ray Jordan, a company spokesman, without providing more details.
Some countries, like China, considered mRNA Covid shots before instead turning to more tried-and-tested technologies, like inactivated virus vaccines. Now, they’re trying to make up for lost time.
A unit of Shanghai Fosun Pharmaceutical Group Co. agreed in May to invest as much as $100 million in a joint venture with BioNTech to make its mRNA vaccine in China. The country is also looking into developing its own expertise in mRNA, with the People’s Liberation Army teaming up with Walvax Biotechnology Co. on a new mRNA shot scheduled to soon go into Phase III trials.
Expensive exercise
In Australia, a research fellow at Melbourne’s Monash Institute of Pharmaceutical Sciences, Harry Al-Wassiti has been investigating mRNA since 2017, and early in the pandemic was collaborating with colleagues on a vaccine. While Australia also initially supported other shots, Monash’s mRNA research is now back in the spotlight with the federal government planning on backing mRNA development.
With support from the state government of Victoria, the institute is readying an mRNA vaccine for trials, possibly in October. “It took a while,” Al-Wassiti said, “but there’s obviously a lot of interest in mRNA.”
Because starting an mRNA vaccine program from scratch is expensive and time-consuming, such initiatives aren’t likely to be of much help in the short-term fight against Covid — unless governments are able to get mRNA technology from existing vaccine makers.
“If you’re not using the license of the originator, you have to go through clinical trials again, and that’s going to add months and months to bringing a vaccine to market,” said Tom Frieden, former director of the Centers for Disease Control and Prevention under the Obama administration and now chief executive officer of Resolve to Save Lives, a public-health initiative that has funding from Bloomberg Philanthropies.
Frieden has worked with industry officials in South Korea, where the government is promoting an mRNA vaccine hub like South Africa’s, in which a foreign vaccine maker will share technology with local companies cooperating on the entire supply chain, from production to delivery.
To make mRNA vaccines more quickly available, developing countries like South Africa, India and Indonesia want the World Trade Organization to waive intellectual property protections for the vaccines. U.S. Trade Representative Katherine Tai endorsed the idea on May 5, but Germany and other European countries are opposed.
Even if a company does agree to transfer its mRNA technology, however, many of these mRNA vaccine plans will need time before they can help save lives.
“I think we should be a bit realistic and give ourselves a couple of years,” said WHO advisor Akanmori. “Two years would be something.” –Bloomberg
Also read: Covid vaccine makers create platform to connect with suppliers to speed up production






