Vaccines against Covid-19 are less effective against the delta variant, a large U.K. study showed in results that may fuel a push for booster shots for fully vaccinated people.
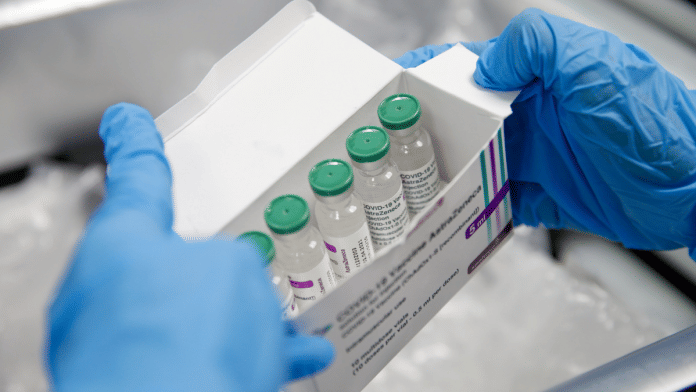
Pfizer Inc. and BioNTech SE’s messenger RNA vaccine lost effectiveness in the first 90 days after full vaccination, though that shot and the one made by AstraZeneca Plc still staved off a majority of Covid infections. When vaccinated people did get infected with delta, they had similar levels of virus in their bodies as those who hadn’t had their shots, backing up a recent assessment by the Centers for Disease Control and Prevention.
The results are likely to fuel calls to give booster shots to the fully vaccinated even as countries around the world still lack enough supply for first immunizations. The U.S. on Wednesday said Americans who got both doses of the Pfizer-BioNTech or Moderna Inc. mRNA vaccine will be able to get a third one after eight months. U.K. authorities are still deciding how broadly boosters should be given. In Israel, which started giving third doses of Pfizer-BioNTech this month, initial results show they have been 86% effective for people over the age of 60.
The U.K. survey, run by the University of Oxford and the Office for National Statistics and published Thursday in a preprint, analyzed more than 3 million PCR tests from a random sample of people for a detailed picture of infection patterns as delta became the dominant variant this year.
“We’re seeing here the real-world data of how two vaccines are performing, rather than clinical trial data, and the data sets all show how the delta variant has blunted the effectiveness of both the Pfizer and AstraZeneca jabs,” said Simon Clarke, an associate professor in cellular microbiology at the University of Reading.
By roughly four and a half months after the second dose, Pfizer’s shot will probably be about on par with Astra’s at preventing infections with a high viral burden, said Koen Pouwels, an Oxford senior researcher who helped lead the study. There wasn’t a statistically significant difference in the Astra shot’s effectiveness over time.
Also read: Why the world may never reach herd immunity against Covid-19
Doubts loom over herd immunity
The results cast further doubt on the possibility of achieving herd immunity via vaccination, said Sarah Walker, a professor of medical statistics and epidemiology at Oxford, who helped lead the study.
“The hope was that unvaccinated people could be protected by vaccinating lots of people,” Walker said. “The higher levels of virus that we’re seeing in these infections in vaccinated people are consistent with the fact that unvaccinated people are just going to be at higher risk, I’m afraid.”
One important piece of the puzzle that’s still missing is data showing how much the vaccines continue to protect against hospitalizations and severe cases of Covid over time, said Penny Ward, a visiting professor in pharmaceutical medicine at King’s College London, who wasn’t involved with the study. The findings may also support giving a booster dose of mRNA vaccine to people who got the Astra shot, which uses a different technology, Ward said in a statement. They also drive home the need for better Covid treatments, she said.
“No vaccine is completely protective against infection with the delta variant,” Ward said. “The low incidence of hospitalization seen to date suggests that in this respect, at least, the vaccines are protecting individuals from developing severe Covid.” —Bloomberg
Also read: Fatigue, loss of smell, lung issues — new study identifies 55 long-term effects of Covid-19