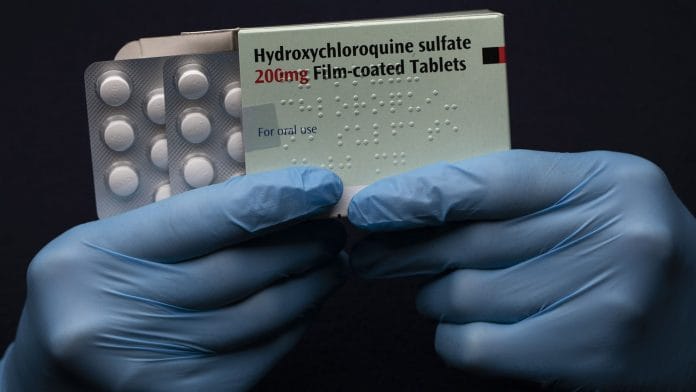
New Delhi: Several questions are being raised about the study published in prominent medical journal The Lancet, which concluded that anti-malarial drug hydroxychloroquine (HCQ) increases risk of death in Covid-19 patients.
The study had prompted the World Health Organization (WHO) to pause clinical trials of HCQ on Covid-19 patients last week, under its giant ‘solidarity trial‘.
Now, more than a hundred scientists and clinicians have raised doubts over the authenticity of the massive hospital database that was the basis of the study.
In an open letter to The Lancet’s Editor-in-Chief Richard Horton and the paper’s authors, the researchers have demanded details about the origin of the data and called for the study to be independently verified by the WHO or another institution.
Infectious disease researchers from Australia have also raised doubts on the study, after they found discrepancies in the data cited.
Hydroxychloroquine or chloroquine, which was touted as a game-changer drug by US President Donald Trump in the fight against coronavirus, was being widely used for the treatment of Covid-19 despite no conclusive evidence of its benefits.
However, the study published on 22 May raised alarm over its aggressive use and showed that the patients receiving HCQ were linked to an elevated risk of death and also experienced increased irregular heart rhythms, when compared to other virus patients.
The large observational study claimed to have analysed data from nearly 96,000 patients. Around 15,000 patients in the study either received HCQ alone or in combination with some antibiotics and was compared to the data of 81,000 controls who did not receive the drug.
Also read: ICMR & Lancet HCQ study aren’t at odds. One is on preventing Covid, other about treating it
What is the discrepancy?
The signatories of the open letter raised doubts about the peer-review process of the study, indicating that it was cleared in a short span of time despite the large dataset.
“The paper, published May 22, included data on over tens of thousands patients hospitalized through April 14, meaning that the authors analyzed the trove of data, wrote the paper and went through the journal’s peer review of its findings in just over five weeks, much faster than usual,” notes a report in The New York Times.
These experts also criticised the methodology used as well as the authors’ refusal to disclose the names of the hospitals where they acquired the data, and the names of the countries they are located in.
A separate investigation by The Guardian found several more discrepancies.
According to the report, the study, which is led by Boston-based Brigham and Women’s Hospital Center for Advanced Heart Disease, had stated that researchers gained access to data from five hospitals in Australia, with 600 Covid-19 patients and 73 deaths as of 21 April.
However, the data from Johns Hopkins University in the US, indicates that Australia had recorded only 67 deaths till 23 April — casting confusion over the original source of the data.
“The federal health department confirmed to Guardian Australia that the data collected on notifications of Covid-19 in the National Notifiable Diseases Surveillance System was not the source for informing the trial,” the report notes.
The discrepancies were established further after the health departments of New South Wales and Victoria in Australia, confirmed that “the study’s results relating to the Australian data did not reconcile with the state’s coronavirus data, including hospital admissions and deaths. The NSW Department of Health also confirmed it did not provide the researchers with the data for its databases.”
Another statistician, Peter Ellis who is a chief data scientist at Nous Group, an international management consultancy, alleged in his personal blog that “the peer-reviewed study that probably used fabricated data”.
“I believe with very high probability the data behind that high profile, high consequence Lancet study are completely fabricated,” he wrote.
“If Surgisphere can name the 671 participating hospitals or otherwise prove that the data is real I will retract that statement, delete this post or write whatever humbling apology they desire. But I think there’s nearly zero chance of that happening,” he added.
Surgisphere is a Chicago-based healthcare data analytics and medical education company that supplied the data for the study.
Also read: Everyone is cherrypicking studies on HCQ. But scientists are divided
Response from authors and data aggregator firm
In response, The Lancet said it had contacted the authors to clarify the discrepancies.
“We have asked the authors for clarifications, we know that they are investigating urgently, and we await their reply,” the scientific journal told Guardian Australia.
The lead author of the study, Dr Mandeep Mehra, was quoted as saying that he had contacted Surgisphere to reconcile the discrepancies with “the utmost urgency”.
Experts also demanded that the data used for analysis be made public or at least opened to an independent statistical review.
However, the response by Surgisphere has cited “privacy reasons” for not being able to share the data.
“We also take data privacy very seriously…Our strong privacy standards are a major reason that hospitals trust Surgisphere and we have been able to collect data from over 1,200 institutions across 46 countries,” the firm said in a statement.
It added, “While our data use agreements with these institutions prevents us from sharing patient level data or customer names, we are able to complete appropriate analyses and share aggregate findings to the wider scientific community. Together, we stand behind the integrity of our studies and our scientific researchers, clinical partners, and data analysts.”
However, it clarified that a hospital was re-classified in their database after it was wrongly identified as an Australian hospital, when in fact it was from Asia. However, it added that “the findings of the paper are unaffected by this update”.
“A hospital that joined the Surgisphere registry on April 1, 2020 self-designated as belonging to the Australasia continental designation. In reviewing the data from each of the hospitals in the registry, we noted that this hospital should have more appropriately been assigned to the Asian continental designation.”
It said that their studies, including the one published in The Lancet, use a registry with data obtained from electronic health records (EHR). “In our hydroxychloroquine analysis, we studied a very specific group of hospitalized patients with COVID-19 and have clearly stated that the results of our analyses should not be over-interpreted to those that have yet to develop such disease or those that have not been hospitalized.”
“We also clearly outlined the limitations of an observational study that cannot fully control for unobservable confounding measures, and we concluded that off-label use of the drug regimens outside of the context of a clinical trial should not be recommended,” it clarified.
Also read: We analysed HCQ risks and benefits, will continue to recommend for prevention: ICMR chief
Effect on trials
The Lancet study had wide-ranging implications and according to an article in British scientific journal Nature, it may also stop people from participating in such trials.
“Researchers have been eagerly awaiting results from clinical trials to yield a clear answer. But now they fear that the Lancet study, and the negative press coverage that followed, might dissuade patients from joining the trials, which would make it even harder to determine whether the drug works against COVID-19,” it said.
However, the enrolments in clinical trials may resume after regulators have been assured that the data from these trials do not indicate that participants are being harmed by HCQ.
Apart from WHO, the UK’s health watchdog Medicines and Healthcare Regulatory Agency (MHRA) has also halted most of the HCQ trials for Covid-19 citing “pending further safety assessments”.
Even in France, the clinical-trial enrolment has been halted and doctors have been forbidden to prescribe the drug outside clinical trials to people with Covid-19.






Since start of Corona India ICMR or other scientists HCQ is supported as benefiting drug for health worker also policemen are provided the drug but in between there many drugs are named and gone aside except HCQ, always remain in lime light.Even the President of USA using the same. then what’s the problem always, “ to be or not to be “ happens about the drug
seems to be business rivalry among pharma companies
Lancet is not the final word in Medicine. The drug has been used for long and long-term for conditions like Rheumatoid Arthritis, almost without any cardiac side effect. Whatever bad complications namely cardiac arrhythmias leading to catastrophic event were not reported in spite of such daily intake for more than five years.
Definitely it’s not just the side effect.
Good that ICMR came out in support of the cheap and easily available locally manufactured drug.
It is beginning to look like the big pharma crowd is ramping up the propagandists in a delusional attempt to downplay a working medicine. The actual data is showing that the hydroxychloroquine medicine is more effective when taken early in the infection cycle.
It is becoming very difficult for us, ordinary citizens, to trust any institution, be it the government, the judiciary, the media, the medical fraternity, anyone. Ideology, money, fame, societal validation etc are making people give up professional ethics.
Why would the American lobbyist funded study promote the use of a drug that’s almost free of cost when an unproven, less effective alternative (Remdesivir) can make them a ton of money?
This research has signatures of LIBRANDUS famous for fabricating data and then presenting it as facts. Librandus always hide behind privacy concerns. If research data can’t be shared publicly, the study can’t be called as research. It looks a propaganda against HCQ that’s largely manufactured in India.