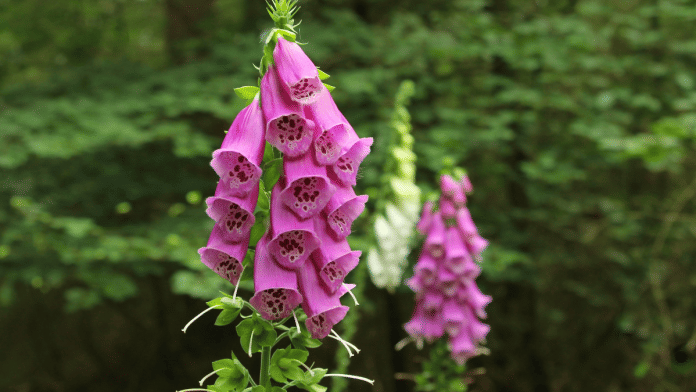
New Delhi: A landmark clinical trial has found that digitoxin, the active ingredient in foxglove plants or digitalis, can be an inexpensive option to treat heart failure, a finding that could have significant implications for developing countries like India.
The DIGIT-HF trial, conducted by German scientists, tracked more than 1,200 participants across three countries over three years and found that digitoxin significantly lowered mortality and hospitalisation rates in patients with reduced heart-pumping function and insufficient emptying of the left ventricle—known in medical terms as HFrEF or heart failure with reduced ejection fraction.
The details of the trial were presented at the European Society of Cardiology Congress 2025 and simultaneously published in The New England Journal of Medicine this month.
Heart failure is a life-threatening cardiovascular condition in which the heart is unable to pump adequate blood to meet the needs of the body.
Though there have been indications that digitoxin, the active ingredient from digitalis, is useful for treating heart failure and has been used for over two centuries, this is the first time its efficacy and safety in managing the condition have been proven scientifically.
Experts said the findings have the potential to establish foxglove as a mainstay for heart failure treatment.
“The findings from the trial are very relevant for our patients. Digitoxin offers benefits on par with costly new therapies, yet at virtually no cost and can be crucial for resource-constrained countries like India,” Dr Ambuj Roy, senior interventional cardiologist with the All India Institute of Medical Sciences (AIIMS), told ThePrint.
Experts said that while digitoxin costs about Rs 2-3 per tablet in India, dapagliflozin, an SGLT-2 inhibitor for heart failure, may cost about 10-20 times more.
Also Read: Experimental drug shows promise in treatment of hard-to-control high blood pressure
Safe, efficacious & cost-effective
Foxglove plants, native to Europe, Western Asia and northwestern Africa, are also used for drug preparations such as digoxin, a compound similar to digitoxin with similar use.
Both digoxin and digitoxin contain cardiac glycosides that increase heart muscle contractility and decrease heart rate by inhibiting the sodium-potassium pump.
Cardiologists say standard medication for heart failure includes beta blockers and inhibitors of the renin-angiotensin-aldosterone system, which relieve the heart, as well as diuretics.
Defibrillators implanted in the patient’s body also help against acute arrhythmias or problems with the rate and rhythm of the heartbeat.
Over the last few years, SGLT-2 inhibitors—drugs that play a crucial role in regulating glucose metabolism by lowering glucose levels through an insulin-independent mechanism and originally meant for treating diabetes mellitus—have also been used to manage heart failure.
But the latest evidence showed that treatment with digitoxin led to a lower combined risk of death from any cause or hospital admission for worsening heart failure compared with a placebo among patients with heart failure and reduced ejection fraction who are on guideline-directed medical therapy.
Dr Jyoti Kusnur, an interventional cardiologist with Manipal Hospital in Goa, explained that, unlike many new therapies, it works by beefing up the heart muscle’s contractility, which can help improve the weakened heart’s ability to pump.
“What is often ignored, however, is its pharmacokinetic profile—instead of being processed in the kidney, digitoxin is metabolised by the liver. So it is of particular use in those with renal impairment, who may have a connection with kidney-metabolised glycosides like digoxin,” the cardiologist said.
Furthermore, digitoxin has a long half-life, which keeps blood levels steady with fewer dosage adjustments, a feature that can help with stable symptom control.
“In carefully selected patients, it can significantly improve the quality of life and reduce symptoms of the condition. The solution is there in careful monitoring and appropriately targeted use to optimise its benefits with the least possible toxicity,” Dr Kusnur said.
(Edited by Sugita Katyal)