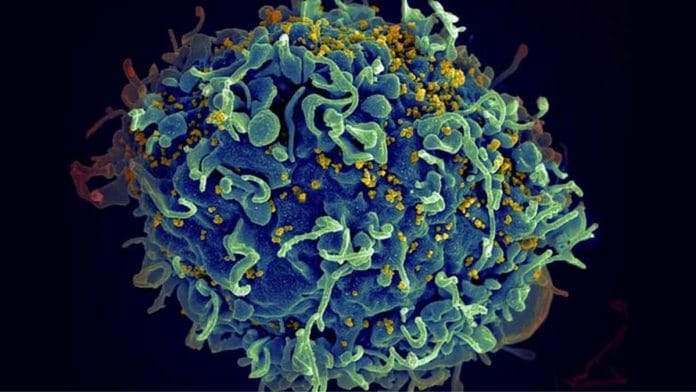
Bengaluru: Eliminating AIDS is a Sisyphian challenge. Treatments mostly miss the Human Immunodeficiency Virus (HIV) that are hidden in the body. But in a breakthrough, a team of researchers from Melbourne have found a way to root out the virus hiding in our immune cells. They claim that they can reach 75 percent of infected cells.
One of the reasons why HIV is a formidable opponent is because it hides inside our cells, making it difficult to eliminate them. The researchers combined different lipids—fats that can deliver treatment into the cell—into a fat bubble to deliver to the right cell where the virus is hidden.
“We sort of took on this challenge to try and see if we could redesign the lipid nanoparticle. And that is eventually where I think the biggest breakthrough has been,” Paula Cevaal, lead author at the University of Melbourne, told ThePrint.
The study, ‘Efficient mRNA delivery to resting T cells to reverse HIV latency’, was published in the Nature Communications journal.
Udayakumar Ranga, a professor at the Jawaharlal Nehru Centre for Advanced Scientific Research (JNCASR), and who was not part of the study told ThePrint, “Even if you have the best weapon in the world, there is nothing you can do to the virus because it is silent.”
The silent virus acts like a sleeper cell
Explaining why it’s so difficult for the body to fight HIV, Ujjwal Rathore, Staff Research Scientist, University of California, said, “Those (virus particles) just look essentially like any other cells which are uninfected (and) your immune system is unable to clear those infected cells.”
Rathore was not part of the study.
Usually to fight the virus, one needs to send mRNA—a messenger to tell the cells what proteins to make—to the cells to activate and kill the virus, a normal procedure in building vaccines. Then the T Cells, a type of white blood cells that fight infection, will be motivated to produce a protein to fight the virus.
Now the challenge is how to deliver that mRNA. The usual delivery of mRNA is not effective as it breaks down by the time it reaches the T cell. “Whereas if you make and encapsulate this mRNA into lipids and lipid nanoparticles, then the stability of mRNA increases, and the delivery is possible into cells,” Rathore added.
Inside the cell, the delivery partner knocks on the door of the T cells. Then the unboxing begins—the endosomal escape mechanism. “(This) will break down the mRNA assembly or the cargo when in contact with the T-cell. Then the mRNA will be released, and that mRNA will start expressing the protein, the targeted protein,” explained Mrinmoy De, Associate Professor, Department of Organic Chemistry, Indian Institute of Science (IISc).
With the help of the newly designed LNP (the delivery partner), the researchers used HIV’s own “master switch” protein—called Tat—to force hidden virus out of dormant immune cells.
The study is carried out by taking cells from humans, in a petri dish inside the laboratory and not on humans. “We haven’t done in this study anything in animal models or anything in people. We’re not there yet,” said Cevaal.
Cevaal’s study showed that one can force the hidden virus out of hiding in infected cells. However, simply revealing the virus is not enough—a second step to boost the immune attacks or adding antiviral drugs will be critical to fully clear the virus.
Imagine the virus is a thief hiding in one of many rooms in a huge palace. To catch the thief, the cops must search every single room. HIV, just like a thief, can hide in any of the CD4, special type of immune cells. So when the war room is highjacked by the HIV sleeper cells, the immunity system collapses.
This is the issue with HIV, which can enter any of the many CD4 cells in the body and hide there. To pop out the stealthy virus, the drug must enter every individual cell, like an encounter specialist.
“Only one in 10,000 to 100,000 CD4 cells may harbour a hidden virus. The therapy of making a drug enter every cell has its undesirable side effects,” said Ranga. According to Ranga the researchers did something smart. They delivered a Tat protein in the form of mRNA and was made to pop into the cells with the help of specially designed LPN.
“However, Tat protein itself is highly toxic and can cause cell death,” Ranga added. So even though they do not activate the cells, the danger remains.
“Of course this is an essential question that we are studying at the moment and that we will continue to study closely. We will perform experiments to test whether they (healthy cells) are affected by the presence of this Tat protein and up to what extent,” Cevaal added.
The potential of such studies depends on how they translate into a technology to reach patients.
“We are very much aware that the pursuit to try and resolve the HIV AIDS pandemic is very much not a done deal, that’s really triggering us to continue working in this area to design a new therapeutic,” Cevaal added.
(Edited by Sanya Mathur)
Also Read: Eradicating malaria or mosquitoes? Gene editing raises ethical questions