New Delhi: In early 2023, doctors at Northwestern Medicine Canning Thoracic Institute in Chicago did something unheard of in medical history—they removed both lungs of a critically ill patient suffering from severe lung disease and kept him alive for two whole days.
The lungs were removed to stop life-threatening infection from spreading and to make the man stable for a double lung transplant. For two days, tubes connected the patient to an artificial lung outside the body. Instead of his own organ, blood was circulated in his body through what is being called a specially designed “total artificial lung” system.
Details of the case were published in Med, a Cell Press journal, last week.
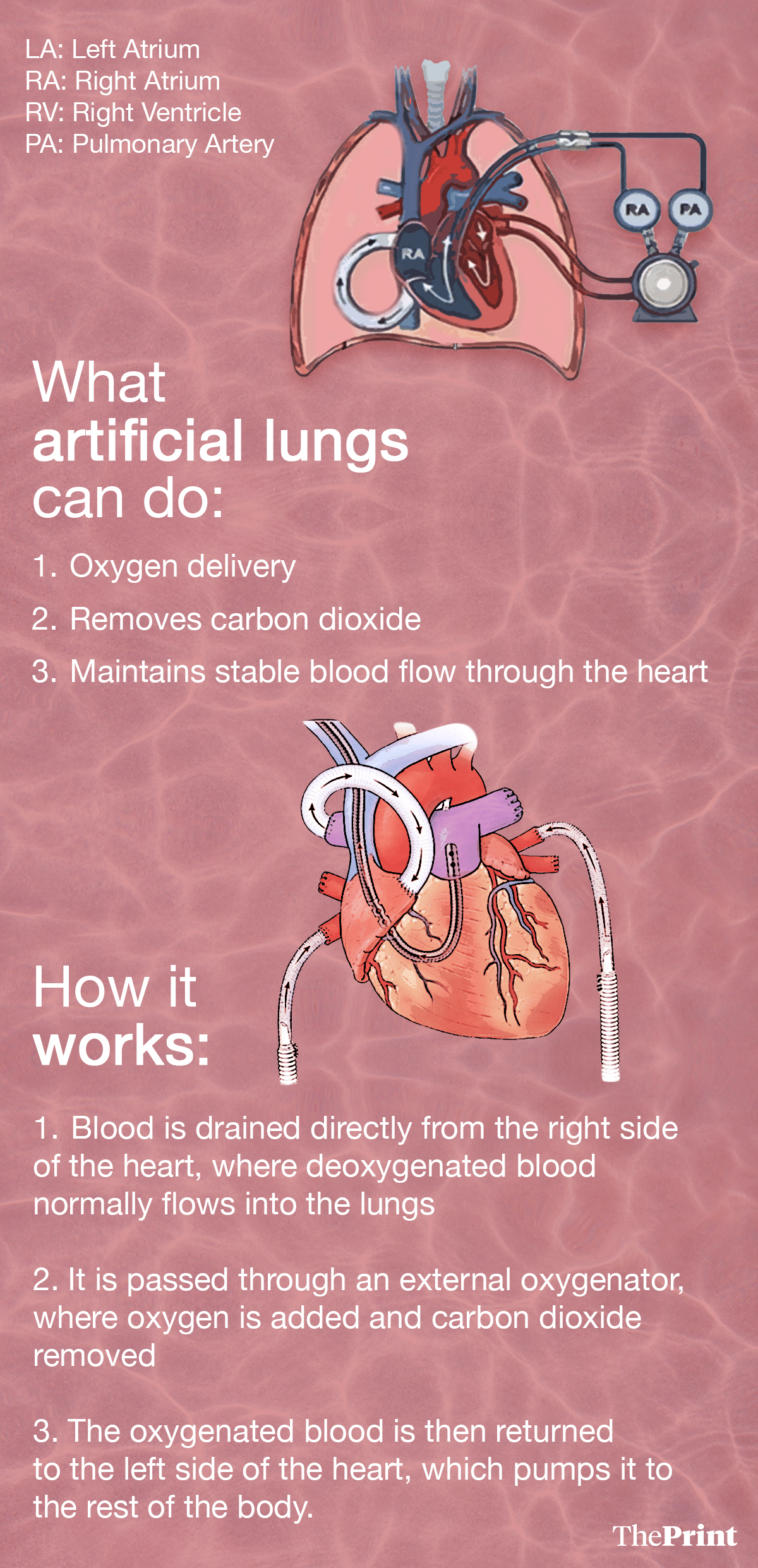
The system took over oxygen delivery, removing carbon dioxide and, most importantly, helped in maintaining stable blood flow through the heart.
Two days later, once donor lungs became available, the patient underwent a lung transplant. Almost three years later, the patient, now in his mid-30s, is back to daily life with “excellent lung function”.
The case has generated a lot of interest in the medical community and given a ray of hope to doctors handling patients with severe lung disease—especially those whose lungs are so infected that keeping them inside the body can pose serious health risks.
The Chicago patient had come with acute respiratory distress syndrome, and the infection had spread rapidly. His lung function deteriorated, followed by failure of the heart and kidneys.
Dr Ankit Bharat, lead author of the case study and a thoracic surgeon at Northwestern Medicine, who performed the 12-hour transplant surgery, told The Washington Post that the patient’s heart had stopped as soon as he arrived in the hospital, and doctors had to perform cardiopulmonary resuscitation (CPR), an emergency procedure used during cardiac or respiratory arrest that involves chest compressions.
The infection was so severe that it caused his lungs to liquify.
The lungs were beyond recovery and were driving infection throughout the body. But the patient was too unstable to undergo an immediate transplant. Doctors performing the surgery faced a dilemma: the lungs had to be removed to control infection, but removing both lungs could lead to the heart collapsing.
To address this, the team at Chicago built a temporary system that could fully replace lung function after both lungs are removed, by helping maintain balanced blood flow through the heart and keep it stable while the body recovered enough to accept a double transplant.
Also Read: With AIIMS Delhi set to train surgeons in face transplant, a look at the procedure & risks involved
‘Total artificial lung’
The system used in Chicago is a device with 25 parts, according to the published study paper and details given out by Dr Bharat. It is a carefully assembled setup that modifies existing extracorporeal (outside the body) life-support technology.
In this system, blood is drained directly from the right side of the heart, where deoxygenated blood normally flows into the lungs. It is passed through an external oxygenator, where oxygen is added and carbon dioxide removed. The oxygenated blood is then returned to the left side of the heart, which pumps it to the rest of the body.
The procedure typically resembles Extracorporeal Membrane Oxygenation (ECMO), a specialised, life-saving but temporary support system for patients with severe, reversible heart or lung failure.
In ECMO, blood is pumped outside the body to a heart-lung machine. This machine removes carbon dioxide and sends oxygen-rich blood back to the body. The blood first flows from the right side of the heart to the machine outside the body, where it is rewarmed and sent back to the body.
ECMO acts as an artificial lung or heart, allowing organs to rest and recover. It is a temporary life support till the time the lung transplant is done.
Dr Arvind Kumar, Chairman of the Institute of Chest Surgery & Lung Transplantation at Medanta Hospital, Gurugram, and Founder & Managing Trustee, Lung Care Foundation, told ThePrint that in standard ECMO, blood is usually drawn from large veins, not directly from the heart.
“The lungs remain inside the body, even if they are not functioning well. In the Chicago case, the lungs were completely removed,” he said.
To prevent the heart from shifting inside the empty chest cavity, surgeons placed temporary saline-filled breast implants on both sides of the chest. These acted as placeholders until donor lungs could be transplanted.
“The heart is supported by the lungs on either side. When you remove both lungs, the heart can shift inside the empty chest cavity. To prevent that, they filled temporary saline-filled implants in both sides of the chest,” Dr Kumar added.
This has been done for the first time, he asserted.
Also Read: The desperate hunt for organ donors in India. Families fight red tape, distrust, ignorance
Chicago case implications
In India, severe lung failure driven by infections is common. Pneumonia, tuberculosis, post-viral lung injury and air-pollution-related diseases together make respiratory illness one of the country’s leading causes of hospitalisation.
According to Global Burden of Disease Study, published in 2018, chronic respiratory diseases accounted for 10% of all deaths in India in 2016.
In such a scenario, doctors say an artificial lung can offer hope, giving doctors a crucial window of two to four weeks to better plan a transplant surgery, shorten recovery time and lead to improved outcomes.
Dr Bharat, whose team operated on the patient in Chicago, told The Post that the artificial lung they have developed represents a “major advance towards a durable and long-term implantable total artificial system”.
The concept of artificial lungs has relevance for infection-driven lung failure, Dr Akshay Budhraja, Senior Consultant, Respiratory & Sleep Medicine at Aakash Healthcare in New Delhi, told ThePrint.
“If such systems become safer and more refined, they could allow doctors to stabilise patients, plan transplants better and reduce emergency procedures,” he said.
According to him, in ECMO, the lungs are still inside. They remain the focus of infection. “Here (Chicago case), the lungs were removed due to infection, so recovery was faster.”
According to Dr Kumar, the Chicago case has changed a long-held assumption that removing both lungs can prove fatal.
“This is very smart thinking and very smart clinical management. It definitely opens up a whole new area for caring for such patients and opens new frontiers for further innovation and progress, which one day may lead to a true total artificial lung,” he said.
Dr Kumar said that nearly 40% of patients on his transplant waiting list die before an organ becomes available. “In a situation like this, a total artificial lung bridge, even for a few days, could help some patients survive until donor lungs are found,” he added.
Dr Budhraja pointed out that a total artificial lung will reduce the cardiac load, and if the technology evolves the way it is hoped—addressing side effects and complications—it could even become a wearable device in the future.
“That may allow patients to be mobile, off ventilators and ECMO, and focus on improving nutrition and correcting deficiencies,” he said.
Machine-assisted lung function is not a new concept, though.
ECMO, for instance, is widely used in intensive care units, including in India. ECMO oxygenates blood outside the body and is used when the lungs fail. But it is designed to temporarily support damaged lungs.
“ECMO works when the lungs are inside the body, even if they are not working,” said Dr Kumar. “Here (Chicago case), the novelty is ECMO with both lungs removed.”
Lungs are not just gas-exchange organs. They regulate blood flow, manage pressure and support heart function. Removing both lungs disrupts circulation. The right side of the heart suddenly has nowhere to pump blood, which can cause immediate heart failure.
The Chicago team of doctors addressed this by creating a flow-adaptive circuit that mimicked lung circulation. Doctors describe this as a “total” artificial lung because it fully replaces lung function, rather than assisting damaged lungs that are still inside the body.
Limitations
Doctors caution that surgery using ‘total artificial lung’ system is unlikely to be used widely, at least in the short run as it is very specialised.
In an article, surgeons at Northwestern Medicine said the procedure requires transplant expertise, advanced life-support systems, round-the-clock multidisciplinary critical care and rapid access to donor organs.
The device used by the Chicago doctors is yet to be used for the second time as the doctors wanted to see how the patient responds in the long term.
Dr Bharat told The Post that the device cannot be tested in clinical trials because it would be unethical to randomise treatment for some dying patients and not for others.
He said that Northwestern Medicine Canning Thoracic Institute will keep a registry that will allow researchers to track how the device performs in other cases.
(Edited by Nida Fatima Siddiqui)
Also Read: Hand transplantation surgeries to now be regulated centrally through a nationwide database