Hyderabad: It takes about twelve years to become a cornea specialist, from an MBBS to an MD to a specialised fellowship. But at the LV Prasad Eye Institute in Hyderabad, a team of doctors is using artificial intelligence to train rural health workers within a year.
Twenty years of electronic patient records, along with imaging specialists who’ve trained computers to spot disease patterns in eye photos, have made this possible.
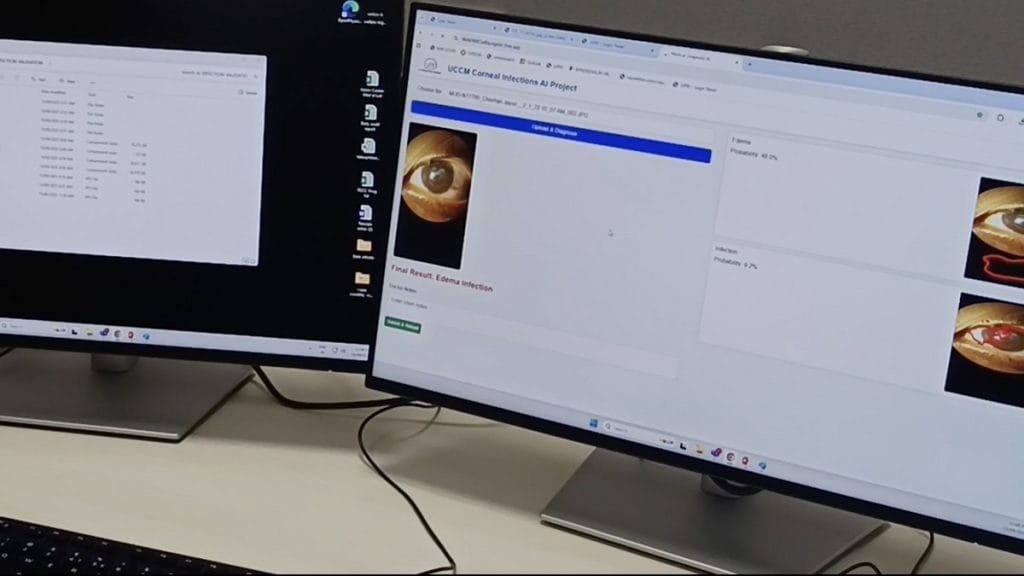
LVPEI has built a set of machine learning models to detect corneal infections. For now, through the institute’s telemedicine system, photos of patients’ eyes are captured and sent to a command centre, where the models are deployed to check for infection. The next step will be to roll them out in primary health centres through a mobile app that lets health workers photograph patients’ eyes, detect issues, and send them to clinicians for review.
The goal is to catch infections early, before they worsen and require surgery or transplants.
At the helm is Dr Pravin Vaddavalli, director of the Shantilal Shanghvi Cornea Institute at LVPEI, leading a team of nine people, including data engineers, clinicians, and image graders.
“We took about 150,000 images of patients who had corneal infections from our archives in LV Prasad Eye Institute. Then a team of data scientists sat down and marked out the areas of interest on these images and then taught the machine that hey, this is how an infection looks,” said Vaddavalli.
The machine learnt over time to detect an infection from a simple photograph
-Dr Pravin Vaddavalli
In a white boardroom with black swivel chairs at LVPEI’s Kismatpur campus, Vaddavalli takes calls from patients hundreds of kilometres away. His goal is to scale up their access to Hyderabad clinicians who cannot visit them physically.
As a corneal disease specialist, his mission is to address the shortage of eye doctors in villages. India sees 20,000 to 25,000 new cases of corneal blindness each year, with rural areas disproportionately affected due to limited eye-care access
“If we enable community health workers to make the right diagnosis using an algorithm that can detect these infections from a simple photograph taken on a mobile phone, we believe that we will empower them with the ability to diagnose these infections early,” he added.

It’s a system where humans and machines work together to bridge longstanding health gaps. The machine learning models — which are yet to be named — flag potential infections that then pass through two layers of checks: first by health workers, then by clinicians.
“We need to train the model to think like a doctor or an ophthalmologist,” said Jagannadha Ganti, chief technology officer, LVPEI. “Nobody knows what happens inside an AI system, but they get an outcome. What we employ is a responsible AI. Along with the outcome, there will be a graphical representation on how the model has arrived at this outcome,”
This is the latest in LVPEI’s attempts to bring artificial intelligence into medical diagnosis. The institute has already tested AI tools to detect glaucoma using smartphone fundus photos and to identify retinoblastoma, an eye cancer, from retinal scans.
“AI models that are developed by medical professionals, based on a real need to provide better diagnosis and treatment, will probably have the most impact on the ground,” said Vaddavalli.
Also Read: Can monkeys teach ‘dumb’ robots? Bengaluru’s CynLr & IISc lab are making automation smarter
AI for an eye
The Reading Room at LVPEI’s five-acre Kismatpur campus doesn’t have any books. Rows of computers stare back at researchers instead. It’s not a place for bibliophiles but a kindergarten for computers learning from humans.
Sushma, a young researcher in her early twenties, shows a computer what a diseased eye looks like. She loads photographs into the system, marks the area of interest, and helps the computer identify spots and colour changes. Each image teaches the system to recognise what infection looks like.
Annotation — selecting an area of interest in an image and telling the computer what to look for — is what helps the AI learn. Researchers feed the model thousands of such images, check the results, and retrain it every time it fails.
“So, the machine learnt over time to detect an infection from a simple photograph,” Vaddavalli said.
The images come with confirmed diagnoses from LVPEI doctors, giving the computer a reliable reference. Ganti, who leads the AI team, said that privacy concerns are factored into the training process. “We de-identify the personally identifiable information, and then pass on the clinical parameters to our AI models.”
On the ground, the model can save patients a lot of time, money, and travel, especially those with limited access to specialists.
Our intention is not to replace our clinicians with AI models. Our intention is to augment and support the clinician’s decision with AI models, to make it faster
-Jagannadha Ganti, CTO, LVPEI
At primary health centres in rural areas, many health workers are not cornea specialists and often struggle to diagnose what they see. Patients also self-treat using over the counter medications or end up with untrained health professionals.
“Sometimes, people try to remove foreign bodies from the eye in unsterile environments and then put a bunch of medicines hoping one of them will work. Most of these therapies result in very severe infections that eventually get referred to larger hospitals and require surgery,” said Vaddavalli.
The solution is to catch corneal issues before they reach that stage through early screening by community doctors and health workers. Since January 2025, the team has used the system on about 1,000 patients through teleophthalmology from LVPEI’s primary care facilities, known as vision centres. There are around 270 such centres across Andhra Pradesh, Telangana, Karnataka, and Odisha.
“If we are able to detect these infections early and prevent them from developing into much more severe infections, we would be able to prevent these patients from requiring a corneal transplant eventually,” Vaddavalli added.
Also Read: India’s 1st commercial quantum computer has a task. Drug development
Humans in the loop
At LVPEI, the machines don’t have the final word. Every diagnosis suggested by the AI goes back to doctors for verification, correction, and feedback.
“Our intention is not to replace our clinicians with AI models. Our intention is to augment and support the clinician’s decision with AI models, to make it faster,” said Ganti.
There’s human input at every stage, from training to application. Each time the AI analyses an image, its results are logged and reviewed by doctors, whose feedback is used to refine the algorithm. This is to ward off any computational errors that the model might make in diagnosing from a photo.
“This is captured for every outcome, for every run of the AI model, and this feedback is used to refine the model’s accuracy going forward. That is how we are building clinician-in-the-loop feedback to reinforce the learning,” said Ganti.
Involving clinicians in the diagnostic process is widely seen as an advantage in healthcare. Studies show that trust in AI systems increases when medical professionals remain part of the decision-making process. For example, in a 2024 policy paper in the Annals of Internal Medicine, the American College of Physicians recommended that AI tools “should be limited to a supportive role in clinical decision-making … since the tools should ideally be used to assist clinicians, not replace them.”
The project also involves training graduates to interpret images and use the mobile application in community health settings.
What our model is trained to do is to pick up from a photo whether the infection is bacterial or fungal. It gives the doctor a head start of about two to three days to start the correct treatment
-Tanmay Nikhil Gokhale, junior ophthalmologist at LVPEI
“We are trying to augment the capacity of these people, to tell them which conditions require immediate care so that they are able to triage cases and send the ones who require a doctor straight to a higher centre,” said Tanmay Nikhil Gokhale, junior ophthalmologist at LVPEI.
Apart from detection, the model classifies the types of corneal infection. Traditionally, a sample would be sent for lab analysis to determine whether the infection is bacterial or fungal, which takes about three days because microbiology labs are far from rural areas, according to Gokhale.

“What our model is trained to do is to pick up from a photo whether the infection is bacterial or fungal. It gives the doctor a head start of about two to three days to start the correct treatment,” he added.
The team is now working to make the ML technology lighter and more adaptable, through a customised language model so it can be used without heavy infrastructure. The larger aim is to extend the model beyond LVPEI to other eye institutes.
“We are still not there yet. It is going to take some time. First of all, we need to build, implement, get output, improvise—and then we will be ready to actually open it up for other institutes to use,” said Ganti.
(Edited by Asavari Singh)






